NTNU, NCFM & ETHOS
Ethos of Scholarship, Academic Integrity & Independence
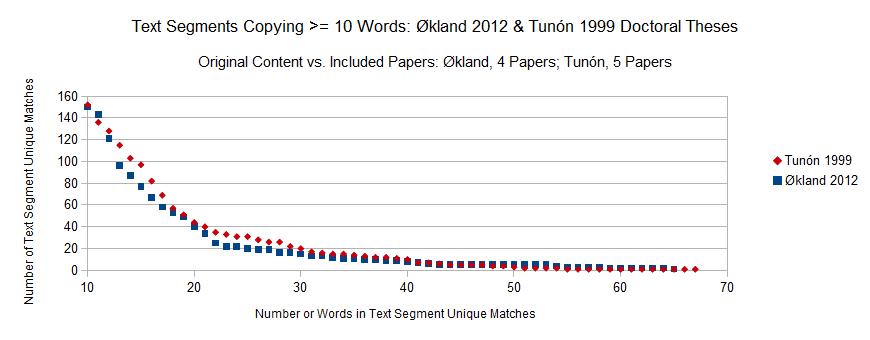
NCFM Supervised: NTNU 1999 PhD Thesis & NTNU 2012 dr.philos. Thesis
NCFM Supervised: NTNU 1999 PhD Thesis & NTNU 2012 dr.philos. Thesis
Inger Økland's 2012 NTNU dr.philos. Thesis (supervised by NCFM eSnurra Group's Sturla H. Eik-Nes, Per Grøttum, and Hakon K. Gjessing) contains incredulous statements regarding Katarina Tunón's 1999 NTNU PhD Thesis (supervised by NCFM Snurra Group's Sturla H. Eik-Nes and Per Grøttum) 13 years earlier. The excerpt below is the statement in Økland's 2012 NTNU dr.philos. Thesis which completely strains credulity.
For example, included below is the expanded excerpt from page 22 of Økland's 2012 NTNU dr.philos. Thesis; an excerpt of 160 words which is so thoroughly wrought with science-bending and conflate-to-obfuscate items they must be numbered and addressed (below).
NCFM Snurra Group's Tunón et al. 2000
The purpose of NCFM eSnurra Group's Tunón et al. 2000 was stated as follows:
An obvious question is: Why did NCFM Snurra Group's Tunón et al. 2000 study decide to use a non-CRL-based GA prediction/estimation model on CRL measurements? More specifically, why did NCFM Snurra Group's Tunón et al. 2000 study use the 'greatest embryonic length' (GEL) model/equation developed in Wisser et al. 1994 instead of NCFM Snurra Group's own Snurra CRL-based GA prediction/estimation model, i.e., their 4th-order polynomial regression model to predict/estimate CRL-based GA from CRL measurements considering that NCFM Snurra Group's own Snurra CRL-based GA prediction/estimation model had been included on the Snurra pregnancy wheel since its 1984 introduction. Moreover, Tunón et al. 2000 stated "BPD was calculated according to the laboratory’s own standard 11," which was the NCFM Snurra Group's BPD-based GA prediction/estimation model, also included on the Snurra pregnancy wheel since its 1984 introduction. So, NCFM Snurra Group's Tunón et al. 2000 study used their own BPD-based GA prediction/estimation model on BPD measurements; however, NCFM Snurra Group's Tunón et al. 2000 study did not use their own CRL-based GA prediction/estimation model on CRL measurements? There is no discussion of this within NCFM Snurra Group's Tunón et al. 2000. However, and again, the more fundamental questions is: Why did NCFM Snurra Group's Tunón et al. 2000 study use the GEL-based GA prediction/estimation model developed in Wisser et al. 1994 for CRL measurements when CRL and GEL are two separate fetal metric measurements. (Source: "Graviditetskalenderen "SNURRA"" Eik-Nes S, Grøttum P. Graviditetskalenderen «SNURRA». Drammen: Scan Med A/S, 1983.)
Importantly, Wisser et al. 1994 stated the reason they used greatest embryonic length (GEL) instead of crown-rump length (CRL) as follows:
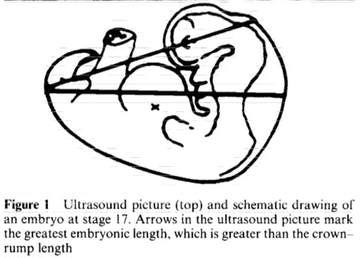
So, it is not surprising Wisser et al. 1994 had neither measured nor modeled CRL because Wisser et al. 1994 had measured and modeled the "greatest embryonic length" (GEL) to predict/estimate GA. GEL is a separate fetal metric, of a different measurement, of a different length than CRL. This is clearly stated in Wisser et al. 1994, with an explanatory GEL vs. CRL measurements diagram (Figure 1, p. 458, included below). [Note: the "ultrasound picture" mentioned in the caption of Figure 1 (below) is not included here because the picture did not reproduce correctly in the online version of Wisser et al. 1994.]
- "Tunón et al. were able to prove that ultrasound dating should be the method of choice even when LMP-data were reliable (Tunón et al. 1996), and in pregnancies conceived after in vitro fertilization (Tunón et al. 2000)." (Source: Inger Økland's 2012 NTNU dr.philos. Thesis, p. 22)
For example, included below is the expanded excerpt from page 22 of Økland's 2012 NTNU dr.philos. Thesis; an excerpt of 160 words which is so thoroughly wrought with science-bending and conflate-to-obfuscate items they must be numbered and addressed (below).
- "In Katarina Tunón's thesis from 1999, 5 studies on different aspects of ultrasound-based pregnancy dating were included (Tunón et al. 1996, Tunón et al. 1998, Tunón et al. 1999b, Tunón et al. 1999a, Tunón et al. 2000), and Snurra was the dating method that was used as the ultrasound-based term prediction model in all the studies. Tunón et al. were able to prove that ultrasound dating should be the method of choice even when LMP-data were reliable (Tunón et al. 1996), and in pregnancies conceived after in vitro fertilization (Tunón et al. 2000). They also stated that there was a tendency towards less precise predictions if the ultrasound examination was carried out earlier than pregnancy week 17–18; the model then estimated the date of delivery too late (Tunón et al. 1998). The authors' assumption was that the term prediction model needed to be improved. To anticipate the course of events; this came about 9 years later (Gjessing et al. 2007)." (Source: Økland's 2012 NTNU dr.philos. Thesis p. 22)
- Contrary to what is stated on page 22 of Økland's 2012 NTNU dr.philos. Thesis, NCFM Snurra Group's Tunón et al. 2000 was not included in Tunón's 1999 NTNU PhD Thesis. In fact, Tunón et al. 2000 is the published version of Tunón et al. Paper V (p. 92-117) in Tunón's 1999 NTNU PhD Thesis. However, after the submission of Tunón et al. Paper V to UOG for publication and after the public defense of Tunón's 1999 NTNU PhD Thesis, someone revised Tunón et al. Paper V in a very strange and dubious way. Specifically, the conclusion of Tunón et al. Paper V was changed, radically, and Figures 1 & 2 of Tunón et al. Paper V, which are scatter plots (or line of identity/equality plots) of IVF-GA vs. CRL-GA at birth/delivery and IVF-GA vs. BPD-GA at birth/delivery, respectively, were replaced with Bland-Altman plots/analyses of GA on the ultrasound date. Thus, the conclusion of Tunón et al. Paper V was radically revised to become the published Tunón et al. 2000.
The radical conclusion change is covered with all the science-bending and conflate-to-obfuscate details further below. The UOG publication history for what was published as Tunón et al. 2000 is as follows: Received 17.11.1998, Revised 20.07.1999, Accepted 23.08.1999. Tunón et al. 2000 was eventually published January 2000 by UOG. Included below are the publication history time intervals for Tunón et al. 2000.
Received to Published: 1 year, 1 month, 2 weeks, 1 day (410 days)
Received to Revised: 8 months, 3 days (244 days)
Revised to Accepted: 1 month, 3 days, (34 days)
Accepted to Published: 4 months, 1 week, 2 days (131 days) - Sturla H. Eik-Nes and Per Grøttum are identified as the supervisors of Tunón's 1999 NTNU PhD Thesis (p. 7). Additionally, Sturla H. Eik-Nes and Per Grøttum are coauthors of all 5 papers included within Tunón's 1999 NTNU PhD Thesis. Moreover, Sturla H. Eik-Nes was President of ISUOG (1998-2002) at the time Tunón et al. Paper V had been submitted, its conclusion radically revised into Tunón et al. 2000 and its publication in Ultrasound in Obstetrics & Gynecology (UOG), also known as The White Journal, the official journal of ISUOG.
- The Tunón et al. 2000 study did not use the NCMF Snurra model to predict/estimate CRL-based GA, as is stated in Økland's 2012 NTNU dr.philos. Thesis. In fact, neither an NCFM Snurra model nor a CRL-base GA model was used in the study of Tunón et al. 2000 (or Tunón et al. Paper V). Instead, and quite strangely, a model-derived equation of the greatest-embryonic-length (GEL) from Wisser et al. 1994 was used, inappropriately and dubiously, with no justification nor explanation as to: 1) why NCFM Snurra Group did not use their own "Snurra" CRL model to predict/estimate CRL-based GA from the historical CRL-measurement data and 2) why NCFM Snurra Group did not use a CRL-based GA model on the historical CRL-measurement data. Moreover, Wisser et al. 1994 make it explicitly clear that greatest embryonic length (GEL) is a different measurement with a different length than the crown-rump length (CRL) measurement. These two measurements are not synonymous as NCFM Snurra Group's Tunón et al. 2000 (or Tunón et al. Paper V) would have readers believe. This episode of science-bending is covered in detail further below. However, it begs the question: How was it possible this blatant science-bending, unethical practice made it past referees' review and editorial review at ISUOG's official journal Ultrasound in Obstetrics & Gynecology (UOG), at the time Strula H. Eik-Nes was President of ISUOG (1998-2002).
- Økland's 2012 NTNU dr.philos. Thesis (p. 22) stated, "...(Tunón et al. 1996, Tunón et al. 1998, Tunón et al. 1999b, Tunón et al. 1999a, Tunón et al. 2000), and Snurra was the dating method that was used as the ultrasound-based term prediction model in all the studies," Økland et al. intentionally and deceptively conflated "ultrasound-based term prediction model" with NCFM Snurra Group's "Snurra" GA prediction/estimation model which used the equivalent of Naegele's rule to calculate (not predict/estimate) EDD from an NCFM Snurra-based GA prediction/estimation. This is a classic example of NCFM eSnurra Group bending science via a conflate-to-obfuscate strategy. The proof Økland et al. knew better is presented 4-pages later on page 26 of Økland's 2012 NTNU dr.philos. Thesis under the heading "eSnurra (‘Trondheim–2007’)" it states: "Conversely, the traditional, sample-based models [Snurra method] use the fetal measurements to estimate the LMP — the EDD is then found by adding a specified number of days to the estimated LMP date [equivalent of Naegele's rule]."
- It is a fact the equivalent of Naegele's rule (i.e., adding a constant number of days, 282 days) was the one and only method used by NCFM Snurra to establish EDD for all 5 studies included in Tunón's 1999 NTNU PhD Thesis. Specifically, NCFM Snurra-based EDD was calculated by simply subtracting the predicted/estimated GA in days on the date of the ultrasound exam from the date of the ultrasound exam to calculate a virtual LMP date (GA day 0 or GA = 0w+0) to which a fixed 282-day gestation period was added to calculate the EDD (or term date). Again, there was no "term prediction model" involved with NCFM Snurra, just a calculation of EDD (or term date) using the equivalent of Naegele's rule.
Importantly, it was July 19, 1998 when the first paper describing the idea, method and benefits of a population-based ultrasound-based term prediction model appeared in the literature, David J. R. Hutchon's Method of Population-based Direct EDD Estimation (PDEE). See: Hutchon 1998, Hutchon & Ahmed 2001 & Hutchon.net. The Hutchon Method of PDEE is Dr. Hutchon's original idea and method for which Dr. Hutchon started his research study in the Department of Obstetrics and Gynaecology, Memorial Hospital, Hollyhurst Road, Darlington, Co. Durham DL3 6HX, UK in 1995, while self-funding all of his own research as he worked full-time as a practicing obstetrician. See: HUTCHON TIMELINE; See: Local Copy of Hutchon 1998 with minor corrections. - Also on page 26 of Økland's 2012 NTNU dr.philos. Thesis, under the heading"eSnurra (‘Trondheim–2007’)" Økland et al. state: "To base a term prediction model on fetal ultrasound measurements from a non-selected population of 36 982 pregnancies (41 343 ultrasound examinations), was a new approach that seemed obvious to statisticians and mathematicians, but not equally obvious to obstetricians." First, Økland et al. have completely changed the definition of an ultrasound-based term prediction model on page 26 from the definition Økland et al used on page 22. In the span of 4 pages, Økland et al. changed the definition of "term prediction model" to the definition that is in fact the Hutchon Method of PDEE, Hutchon 1998.
Second, Økland et al. state NCFM eSnurra "was a new approach" when it is an incontrovertible fact that Dr. Hutchon's seminal Hutchon 1998 of his original idea and method, the Hutchon Method of PDEE, had been published on 19.07.1998, 13 years, 5 months, 3 weeks, 4 days (or 4,926 days) before the public defense and publication of Økland's 2012 NTNU dr.philos. Thesis on 13.01.2012; and, 11 years, 4 months, 3 weeks, 1 day (4,163 days) before the publication of Salomon et al. 2010 on 11.12.2009 [plagiarized Dr. Hutchon's original idea and method, the Hutchon Method of PDEE]; and, 8 years, 10 months, 2 weeks, 6 days (or 3,246 days) before the publication of NCFM eSnurra Group's Gjessing et al. 2007 on 08.06.2007; and, 7 years, 1 month, 2 weeks, 6 days (or 2,608 days) before the publication of NCFM eSnurra Group's Eik-Nes et al. 2005 on 08.09.2005; and, 2 years, 6 months, 1 week, 6 days (or 928 days) before the publication of Taipale & Hiilesmaa 2001 on 01.02.2001. [Taipale & Hiilesmaa 2001 was a recognized Norway-Finland collaboration project with NCFM Snurra Group who plagiarized Dr. Hutchon's original idea and method, the Hutchon Method of PDEE. Interestingly, the lead author, Pekka Taipale, was employed to work at NCFM by Sturla H. Eik-Nes of NCFM Snurra Group. Uncharacteristically, Sturla H. Eik-Nes and Per Grøttum forewent authorship credit on Taipale & Hiilesmaa 2001.]
Also, NCFM eSnurra Group ignored a letter dated 26.07.2007 from Dr. Hutchon regarding NCFM eSnurra Group's appropriation and plagiarism of his original idea and method in their Gjessing et al. 2007; a letter Håkkon K. Gjessing, the corresponding author, has acknowledged he received.
Moreover, and while Økland et al. and NCFM eSnurra Group had been aware of Dr. Hutchon's seminal Hutchon 1998, Hutchon & Ahmed 2001 & Hutchon.net, all have remained individually and collectively silent regarding the blatant ongoing research misconduct via plagiarism by NCFM eSnurra Group. - Økland et al. stated (p. 26) that a population-based EDD estimation "seemed obvious to statisticians and mathematicians, but not equally obvious to obstetricians." However, Økland et al. and NCFM eSnurra Group knew Dr. David J. R. Hutchon was a practicing obstetrician when he developed his ordinal idea and method, the Hutchon Method of Population-based Direct EDD Estimation (PDEE). This fact is made clear in his publications and website (Hutchon 1998, Hutchon & Ahmed 2001 & Hutchon.net); publications which Økland et al. had read and cited 11 separate times in Økland's 2012 NTNU dr.philos. Thesis, but neither Økland et al. nor NCFM eSnurra Group have ever cited Dr. Hutchon for his original idea and method, the Hutchon Method of PDEE, which, of course.
Incredibly, Økland's 2012 NTNU dr.philos. Thesis cited Dr. Hutchon 11 times, but only for peripheral items associated with LMP and selection bias; topics for which NCFM eSnurra Group could have cited themselves. Citing Dr. Hutchon 11 times, but not citing him for his original idea and method, the Hutchon Method of PDEE, required significant forethought and effort by Økland et al. and NCFM eSnurra Group. Strangely (or, clearly, not so strangely) Økland et al. and NCFM eSnurra Group have never once cited, credited, acknowledged or communicated with Dr. Hutchon in any way, whatsoever, with respect to his original idea and method, the Hutchon method of PDEE; the idea and method NCFM eSnurra Group appropriated as their own original idea and method and then plagiarized in NCFM eSnurra Group's Eik-Nes et al. 2005 and Gjessing et al. 2007, and many subsequent publications. Consequently, NCFM eSnurra Group is presently engaged in what is now 13-years of ongoing research misconduct via plagiarism. - Moreover, Økland's 2012 NTNU dr.philos. Thesis was acknowledged and promoted as independent academic justification by Directorate of Health for their selection of the suboptimal, unilateral ultrasound-based NCFM eSnurra pregnancy-dating "method" (i.e., the appropriated, plagiarized, misused Hutchon Method of PDEE) for national implementation, against the explicit, published warnings of the risks and consequences by Norway's obstetric & fetal medicine experts. In fact, Økland's 2012 NTNU dr.philos. Thesis is the only document used by Directorate of Health to make their selection which is publicly available; and, it is publicly available due to the law, not Directorate of Health. Consequently, NCFM eSnurra Group and Directorate of Health engaged in bending policy-relevant science to bend national obstetric & fetal medicine policy, the effect of which was the implementation of a suboptimal, national obstetric & fetal medicine policy which is proven to cause increased medical risks, critical medical mistakes and grievous medical harms (including perinatal death) for some of Norway's women and their fetuses/babies. This is a stone-cold fact, not an opinion.
- Økland's 2012 NTNU dr.philos. Thesis (p. 22) repeated the science-bending, conflate-to-obfuscate strategy by stating "The authors' assumption was that the term prediction model needed to be improved." Again, it is a fact NCFM Snurra Group did not have a "term prediction model...to be improved." Again, the equivalent of Naegele's rule was the one and only method used to calculate EDD from a prediction/estimation of GA for all 5 studies included in Tunón's 1999 NTNU PhD Thesis. The one and only GA prediction/estimation model used for all 5 studies included in Tunón's 1999 NTNU PhD Thesis was NCFM Snurra Group's Snurra model (i.e., with the exception of the inappropriate, science-bending, unethical use of the GEL-based GA model from Wisser et al. 1994 on CRL measurement data in Tunón et al. Paper V, which was revised to be published later as Tunón et al. 2000. It is important to understand that the NCFM Snurra Group's "Snurra" model was an implementation of the Campbell Method of Gestational Age Estimation, Campbell 1969, just as NCFM eSnurra Group's "eSnurra" model was an implementation of the Hutchon Method of PDEE, Hutchon 1998. [See: GA & EDD Methods]
- Moreover, it simply was not possible for NCFM Snurra Group to have used an "ultrasound-based term prediction model" to predict/estimate EDD because NCFM Snurra Group did not have an EDD prediction/estimation model based on all the required historical pregnancy data: 1) ultrasound date, 2) actual birth/delivery date and 3) the associated set of ultrasound-based fetal metric measurements and other variables. In short, NCFM Snurra Group had not yet appropriated and plagiarized the Hutchon Method of Population-based Direct EDD Estimation (PDEE) and they had not yet collected and assembled the necessary data to build and train models which would later (i.e., after the appropriation of the Hutchon Method) come to be known as NCFM eSnurra.
- However, and strangely (or, clearly, not so strangely), Neither Økland et al. nor NCFM eSnurra Group ever cited Dr. Hutchon for his Hutchon Method of Population-based Direct EDD Estimation (PDEE). Citing Dr. Hutchon 11 times and intentionally excluding Dr. Hutchon from any association with his original idea and method of PDEE, required significant forethought and effort by Økland. A larger insult to Dr. Hutchon could not have been engineered., i.e., other than NCFM eSnurra Group's ongoing research misconduct via plagiarism. Moreover, Økland, as a member of NCFM eSnurra Group, remained completely silent about the appropriation and plagiarism of the Hutchon Method of PDEE in NCFM eSnurra Group's Gjessing et al. 2007, plagiarism which she continued throughout her 2012 NTNU dr.philos. Thesis and the 4 papers included therein and published in UOG, all of which were coauthored by the other NCFM eSnurra Group members which included Sturla H. Eik-Nes, then a former President of ISUOG (1998-2002).
- The same science-bending, conflate-to-obfuscate strategy is used by NCFM eSnurra Group today, however, it has been inverted in order to conflate direct EDD prediction/estimation via NCFM eSnurra (via the Hutchon Method of PDEE) with the use of Naegele's rule, in reverse, to establish a calculated (not predicted/estinated) GA. Specifically, GA is calculated by NCFM eSnurra Group by subtracting 282 (or 283) days from the predicted/estimated EDD date to calculate a virtual LMPD (GA day 0, 0w+0). There is no GA prediction/estimation model involved, despite NCFM eSnurra Group's published claims that their "method" estimates GA. NCFM Snurra/eSnurra Groups' science-bending, conflate-to-obfuscate strategy appears to have originated with Tunón's 1999 NTNU PhD Thesis and, most specifically, with the radical, science-bending, conflate-to-obfuscate change to the conclusion of Tunón et al. Paper V in Tunón's 1999 NTNU PhD Thesis to created what was subsequently published as NCFM Snurra Group's Tunón et al. 2000, which had been received by UOG for publication on 17.11.1998, 4 months after the publication of Hutchon 1998 on 19.07.1998.
NCFM Snurra Group's Tunón et al. 2000
The purpose of NCFM eSnurra Group's Tunón et al. 2000 was stated as follows:
- "The aim of this study was to compare gestational age assessed from the time of in vitro fertilization with the gestational age calculated for the ultrasonic measurement of the CRL and the BPD in pregnancies conceived after in vitro fertilization." (Source: Tunón et al. 2000, p. 41)
- "Gestational age according to CRL was calculated by the equation developed by Wisser derived from pregnancies conceived after assisted reproductive techniques:
t = 35.72 + 1.082L^(1/2) + 1.472L - 0.09749L^(3/2)
where L is the greatest embryonic length 10. Gestational age according to the BPD was calculated according to the laboratory’s own standard 11." (Source: "Gestational age in pregnancies conceived after in vitro fertilization: a comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter" K. TUNON, S.H. EIK-NES, P. GRØTTUM, V. VON DURING and J.A. KAHN. Ultrasound Obstet Gynecol 2000; 15: 41–46,. p. 42. Received 17-11-98, Revised 20-7-99, Accepted 23-8-99) [Note: Citation 10: Estimation of gestational age by transvaginal sonographic measurement of greatest embryonic length in dated human embryos Wisser J, Dirschedl P, Krone S. Ultrasound Obstet Gynecol, 1994]
An obvious question is: Why did NCFM Snurra Group's Tunón et al. 2000 study decide to use a non-CRL-based GA prediction/estimation model on CRL measurements? More specifically, why did NCFM Snurra Group's Tunón et al. 2000 study use the 'greatest embryonic length' (GEL) model/equation developed in Wisser et al. 1994 instead of NCFM Snurra Group's own Snurra CRL-based GA prediction/estimation model, i.e., their 4th-order polynomial regression model to predict/estimate CRL-based GA from CRL measurements considering that NCFM Snurra Group's own Snurra CRL-based GA prediction/estimation model had been included on the Snurra pregnancy wheel since its 1984 introduction. Moreover, Tunón et al. 2000 stated "BPD was calculated according to the laboratory’s own standard 11," which was the NCFM Snurra Group's BPD-based GA prediction/estimation model, also included on the Snurra pregnancy wheel since its 1984 introduction. So, NCFM Snurra Group's Tunón et al. 2000 study used their own BPD-based GA prediction/estimation model on BPD measurements; however, NCFM Snurra Group's Tunón et al. 2000 study did not use their own CRL-based GA prediction/estimation model on CRL measurements? There is no discussion of this within NCFM Snurra Group's Tunón et al. 2000. However, and again, the more fundamental questions is: Why did NCFM Snurra Group's Tunón et al. 2000 study use the GEL-based GA prediction/estimation model developed in Wisser et al. 1994 for CRL measurements when CRL and GEL are two separate fetal metric measurements. (Source: "Graviditetskalenderen "SNURRA"" Eik-Nes S, Grøttum P. Graviditetskalenderen «SNURRA». Drammen: Scan Med A/S, 1983.)
Importantly, Wisser et al. 1994 stated the reason they used greatest embryonic length (GEL) instead of crown-rump length (CRL) as follows:
- "The measurement of greatest length was preferred to crown-rump length because of difficulties in defining the cranial reference point in the embryo before 42 days after the last menstrual period 17." (p. 458) (Source: "Estimation of gestational age by transvaginal sonographic measurement of greatest embryonic length in dated human embryos" Wisser J, Dirschedl P, Krone S. Ultrasound Obstet Gynecol, 1994)
So, it is not surprising Wisser et al. 1994 had neither measured nor modeled CRL because Wisser et al. 1994 had measured and modeled the "greatest embryonic length" (GEL) to predict/estimate GA. GEL is a separate fetal metric, of a different measurement, of a different length than CRL. This is clearly stated in Wisser et al. 1994, with an explanatory GEL vs. CRL measurements diagram (Figure 1, p. 458, included below). [Note: the "ultrasound picture" mentioned in the caption of Figure 1 (below) is not included here because the picture did not reproduce correctly in the online version of Wisser et al. 1994.]
As stated in Wisser et al. 1994:
Consequently, NCFM Snurra Group's Tunón et al. 2000 study acquired a polynomial regression model/equation from Wisser et al. 1994 which had been fitted by regressing on GEL measurements, not CRL measurements, to estimate GA and then used the GEL-based model, knowingly, to estimate GA for CRL measurements. Ergo, and not surprisingly, and with GEL being a longer length measurement than CRL, a GEL-based GA estimate of a CRL measurement would tend to underestimate GA. Moreover, there was no discussion of this fundamental, methodological "issue" in NCFM Snurra Group's Tunón et al. 2000. Moreover, Wisser et al. 1994 (p. 457) reported:
Similarly, IVF-CRL systematic error (mean = 0.9, bias) i.e., GEL-based CRL-GA underestimated IVF-based GA by 0.9 days on average due, or partially due, to the GEL model/equation applied, inappropriately, to CRL measurements to estimate GA. The induced bias would manifest as increased systemic error (mean = 0.9, bias). The key question is: How much GEL model/equation bias was induced? Any reduction in the IVF-CRL pair's systematic error (mean = 0.9, bias) would result in a simultaneous decrease in NCFM Snurra Group's BPD-based GA estimation accuracy in the second-trimester relative to CRL-based GA estimation accuracy in the first-trimester; after all, Tunón et al. 2000 was a methods comparison study.
However, elimination or reduction of IVF-CRL systematic error would have been inconvenient to NCFM Snurra Group's agenda; an agenda of NCFM Snurra BPD-based GA & EDD assignments at the second-trimester, 18wUSE and not first-trimester CRL-based GA & EDD assignments, regardless of whose model or model type (GEL or CRL) was used. Ergo, NCFM Snurra BPD-based GA appeared problematic.
Someone or some group could not have planned a better way to intentionally induce bias into the comparisons of: 1) IVF-GA vs. CRL-GA and 2) BPD-GA vs. CRL-GA in order to effect the results of:
As reported in NCFM Snurra Group member Inger Økland's 2012 NTNU dr.philos. Thesis, NCFM Snurra Group had been well aware BPD underestimated "fetal age with BPD measurements" from the results of both an internal study and external study.
NCFM Snurra Group's Tunón et al. 2000 Abstract conclusion stated, incredulously, CRL-based GA and BPD-based GA estimates were of "equally high agreement." Apparently, NCFM Snurra Group had engaged in doublethink where: 2 + 2 = 5.
NCFM Snurra Group's Tunón et al. 2000 originated as "Paper V" in Tunón's 1999 NTNU PhD Thesis, supervised by NCFM Snurra group members Sturla H. Eik-Nes and Per Grøttum; published after Tunon's public defense as: "Gestational age in pregnancies conceived after in vitrofertilization: a comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter" K. TUNON, S.H. EIK-NES, P. GRØTTUM, V. VON DU¨RING and J.A. KAHN. Ultrasound Obstet Gynecol 2000; 15: 41–46. However, the Discussion section conclusion had been changed, radically, after Tunon's public defense and before "Paper V" was published in Ultrasound in Obstetrics & Gynecology (UOG), the official journal of the International Society of Ultrasound in Obstetrics and Gynecology, of which Sturla H. Eik-Nes was President (1998-2002) at the time.
Closing the Department of the Redundancy Department with Obvious Biological Knowledge
Bergen Group made the point of using "obvious biological knowledge" to end the dubious practice of using suboptimal, unilateral ultrasound-based pregnancy dating to date assisted fertilization pregnancies.
In his seminal article, Bergh 1992, in Tidsskrift for den Norske legeforening, Dr. Johan Bergh reported on 31 perinatal deaths (7.7% in 1991), a notable increase from the prior year (4.2% in 1990) at Rogaland Hospital in Stavanger, Norway. All 31 perinatal deaths had their EDD, which had been established using Naegele's rule, postponed by ultrasound. One of the deaths Dr. Bergh reported resulted after a woman who had become pregnant via in vitro fertilization (IVF) had her factual IVFD-based EDD postponed by 22 days with an NCFM Snurra BPD-based GA from which the woman's EDD had been calculated using Naegele's rule. This was done in accordance with Directorate of Health's 'TUL' policy with their protocol of evidence-obviated medicine. Think about this. A woman's factual in vitro fertilization date (IVFD), the actual definition of GA, had been obviated from all medical evidence to ensure NCFM Snurra Group "estimated" the woman's GA using ultrasound via NCFM Snurra Group's BPD-based GA model and, therefrom, calculate an EDD using Naegele's rule. Again, and to be absolutely clear, the woman's GA did not need to be estimated by ultrasound, as it had already been established, exactly, via in vitro fertilization and her IVFD. Again, IVFD is the definition of GA; it is the 'gold standard' of GA which is used as the reference standard in clinical studies to compare fetal biometry prediction/estimation methods. The 'TUL' policy and protocol of evidence-obviated medicine caused the grossly inaccurate NCFM Snurra BPD-based GA & EDD to be used, which created sub-optimal obstetric and fetal awareness; which caused sub-optimal obstetric and fetal management, which caused increased medical risks, critical medical mistakes and grievous medical harms; risks, mistakes & harms which included perinatal death. Which begs the obvious question: Since the inception of 'TUL' how many times has this happened and, how many times has this resulted in perinatal death? Included below is an excerpt from Bergh 1992.
It appears clear Ministry of Health and Care Services, Directorate of Health and NCFM Snurra Group believed women of IVF pregnancies (and their doctors and midwives) were somehow mathematically challenged and needed an NCFM Snurra BPD-based GA in order to help women of IVF pregnancies (and their doctors and midwives) add 266 (or 268) days to their IVFD or add 280 (or 282) days to their virtual LMPD. Included below is the: 1) calculation from NCFM Snurra BPD-based GA for EDD and 2) calculation from IVFD for EDD. Color text was used to highlight the corresponding similarities and differences between these simple calculations. [Note: Has your head recovered?]
Nevertheless, somehow Tunón et al. 2000 found its way (or was guided) through the referees' and editors' reviews and then published in Ultrasound in Obstetrics & Gynecology (UOG) also know as The White Journal, the official journal of the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) of which Sturla H. Eik-Nes was President (1998-2002) at the time, as well as Principal Supervisor of Tunón's 1999 NTNU PhD Thesis and a Tunón et al. 2000 coauthor. Moreover, and again, Tunón et al. 2000 was published with 2 entirely different conclusions, the Abstract conclusion and the Discussion section conclusion, neither of which was supported by the study's data. Moreover, the Discussion section conclusion conflated NCFM Snurra Group's ability to estimate gestational age and NCFM Snurra Group's then nonexistent capability to estimate day/date of delivery (EDD) i.e., via the Hutchon Method of Population-based Direct EDD Estimation (PDEE) (Hutchon, 1998). The reason the capability was non-existent is because NCFM Snurra/eSnurra Group had not appropriated, plagiarized and misused the Hutchon Method of PDEE until later. And, at the same time, 1999, Dr. Hutchon had submitted a more robust manuscript of the Hutchon Method of PDEE to Ultrasound in Obstetrics & Gynecology (UOG), received by UOG 13.07.1999 and coded as UOG 99/155.
Ironically, NCFM Snurra Group's Tunón et al. 2000 is among the 4 cited references "(11-14)" in the excerpt below, taken from page 2 of: COMMITTEE OPINION Number 700, described in the source reference below.
Regarding standard deviation (SD), Tunón et al. 2000 stated:
- "The aims of our study were to assess the accuracy of embryonic age estimation and construct dating curves based on the greatest embryonic length. A prerequisite for precise ultrasonographic determination of gestational age in the antenatal care clinic is the availability of monograms derived from dated embryos." (p. 457) (Source: "Estimation of gestational age by transvaginal sonographic measurement of greatest embryonic length in dated human embryos" Wisser J, Dirschedl P, Krone S. Ultrasound Obstet Gynecol, 1994)
Consequently, NCFM Snurra Group's Tunón et al. 2000 study acquired a polynomial regression model/equation from Wisser et al. 1994 which had been fitted by regressing on GEL measurements, not CRL measurements, to estimate GA and then used the GEL-based model, knowingly, to estimate GA for CRL measurements. Ergo, and not surprisingly, and with GEL being a longer length measurement than CRL, a GEL-based GA estimate of a CRL measurement would tend to underestimate GA. Moreover, there was no discussion of this fundamental, methodological "issue" in NCFM Snurra Group's Tunón et al. 2000. Moreover, Wisser et al. 1994 (p. 457) reported:
- "Recent studies on measurements of crown-rump length in pregnancies with known date of ovulation 12, 14 show an underestimation of gestational age by conventional dating curves 5, 10."
- "It has been shown that CRL dating curves based on the last menstrual period underestimate the gestational age compared to dating curves based on known ovulation date 15."
Similarly, IVF-CRL systematic error (mean = 0.9, bias) i.e., GEL-based CRL-GA underestimated IVF-based GA by 0.9 days on average due, or partially due, to the GEL model/equation applied, inappropriately, to CRL measurements to estimate GA. The induced bias would manifest as increased systemic error (mean = 0.9, bias). The key question is: How much GEL model/equation bias was induced? Any reduction in the IVF-CRL pair's systematic error (mean = 0.9, bias) would result in a simultaneous decrease in NCFM Snurra Group's BPD-based GA estimation accuracy in the second-trimester relative to CRL-based GA estimation accuracy in the first-trimester; after all, Tunón et al. 2000 was a methods comparison study.
However, elimination or reduction of IVF-CRL systematic error would have been inconvenient to NCFM Snurra Group's agenda; an agenda of NCFM Snurra BPD-based GA & EDD assignments at the second-trimester, 18wUSE and not first-trimester CRL-based GA & EDD assignments, regardless of whose model or model type (GEL or CRL) was used. Ergo, NCFM Snurra BPD-based GA appeared problematic.
Someone or some group could not have planned a better way to intentionally induce bias into the comparisons of: 1) IVF-GA vs. CRL-GA and 2) BPD-GA vs. CRL-GA in order to effect the results of:
- CRL-GA appearing worse than reality, relative to IVF-GA
- BPD-GA appearing better than reality, relative to CRL-GA.
As reported in NCFM Snurra Group member Inger Økland's 2012 NTNU dr.philos. Thesis, NCFM Snurra Group had been well aware BPD underestimated "fetal age with BPD measurements" from the results of both an internal study and external study.
- "A new dating method, shown in Figure 10, was introduced in 2004. The occasion was in part the results of a study by Kiserud and Rasmussen (1999), that confirmed the findings by Tunón et al. (1998), that Snurra underestimated fetal age with BPD measurements before pregnancy week 17–18 (Figure 11)." (Source: Økland 2012 NTNU dr.philos. Thesis, p. 23)
- "The normal range curve underestimated the BPD in the lower part of the interval at 15-22 gestational weeks and overestimated the BPD in the upper part of the interval. The variance in the distribution cannot be examined, as the number of examinations, both in the lower and the upper part of the prediction interval, was too low to compare the influence of age on the method." (Source: "The impact of fetal, maternal and external factors on prediction of the day of delivery by the use of ultrasound" K. Tunon, S. H. Eik-Nes and P. Grøttum. Ultrasound Obstet Gynecol 1998;11:99-103, p. 102)
- "The gestational age at the ultrasound examination influenced the difference between the day of delivery and the predicted day. An ideal prediction method should not be influenced by the gestational age at the examination. The normal range curve underestimated the BPD in the lower part of the interval at 15-22 gestational weeks and overestimated the BPD in the upper part of the interval." (Source: "The impact of fetal, maternal and external factors on prediction of the day of delivery by the use of ultrasound" K. Tunon, S. H. Eik-Nes and P. Grøttum. Ultrasound Obstet Gynecol 1998;11:99-103, p. 102)
- "This evaluation confirmed the underestimation of fetal age if Trondheim–1984 [NCFM Snurra] was used in early second-trimester predictions and they concluded that the new reference values more precisely assessed GA." (Source: Økland 2012 NTNU dr.philos. Thesis, p. 25)
- The NCFM Snurra BPD underestimation problem was identified by Drs. Kiserud and Rasmussen of Bergen Group. (Source: "Terminbestemmelse ved hjelp av ultralyd – kan metoden bli bedre?" Kiserud T, Rasmussen S. Tidsskr Nor Lægeforen 1999;29:4331-4)
- An obvious question is: Had the NCFM Snurra BPD estimation problems been known to NCFM Snurra Group prior to "the findings by Tunón et al. (1998)" as reported in Økland's 2012 NTNU dr.philos. Thesis?
- there was a problem with NCFM Snurra (or Trondheim–1984) BPD-based GA underestimating GA,
- the GEL-based model/equation from Wisser et al. 1994 used on CRL measurements to estimate GA (inappropriately) in NCFM Snurra Group's Tunón et al. 2000 study would underestimate CRL-based GA,
- since Tunón et al. 2000 was a methods comparison study of CRL-based GA & BPD-based GA relative to IVF-based GA reference standard, i.e., actual GA, NCFM Snurra BPD-based GA would not appear to be as problematic relative to the bias-inducing GEL-based model/equation estimations of CRL-based GA.
NCFM Snurra Group's Tunón et al. 2000 Abstract conclusion stated, incredulously, CRL-based GA and BPD-based GA estimates were of "equally high agreement." Apparently, NCFM Snurra Group had engaged in doublethink where: 2 + 2 = 5.
NCFM Snurra Group's Tunón et al. 2000 originated as "Paper V" in Tunón's 1999 NTNU PhD Thesis, supervised by NCFM Snurra group members Sturla H. Eik-Nes and Per Grøttum; published after Tunon's public defense as: "Gestational age in pregnancies conceived after in vitrofertilization: a comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter" K. TUNON, S.H. EIK-NES, P. GRØTTUM, V. VON DU¨RING and J.A. KAHN. Ultrasound Obstet Gynecol 2000; 15: 41–46. However, the Discussion section conclusion had been changed, radically, after Tunon's public defense and before "Paper V" was published in Ultrasound in Obstetrics & Gynecology (UOG), the official journal of the International Society of Ultrasound in Obstetrics and Gynecology, of which Sturla H. Eik-Nes was President (1998-2002) at the time.
- "Conclusion" section within the Summary of Tunón's 1999 NTNU PhD Thesis (p. 9-11) states:
"Assessment of gestational age; from the time of IVF, and from measurements of CRL or BPD in pregnancies conceived after in vitro fertilization shows high agreement between the three methods. This supports the use of ultrasound as a reliable method for estimation of gestational age. The ultrasound method can therefore be recommended as the method of choice for dating pregnancies." - Before Publication, After Public Denfense: Discussion Conclusion: Tunón et al. Paper V (p. 13) Tunón's 1999 NTNU PhD Thesis
"In spite of the fact that IVF pregnancies are achieved through intervention, the high agreement between the gestational age calculated from the time of IVF and from the early CRL measurements in the same pregnancies, the high agreement between gestational age calculated from the time of IVF and BPD supports the use of ultrasound as a reliable method for estimation of gestational age." - After Publication: Discussion Conclusion: Tunón et al. 2000 (p. 45)
"In spite of the fact that IVF pregnancies are achieved through intervention, the high agreement between the gestational age calculated from the time of IVF and from the early CRL measurements in the same pregnancies, the high agreement between gestational age calculated from the time of IVF and BPD supports the use of ultrasound as a reliable method for estimation of day of delivery both in normally conceived pregnancies and IVF pregnancies." [Note: Yes, your head just exploded; it has that effect. You will recover, then read it again, but no more than twice within 1 hour; the brain has cognitive trauma limits.] (Source 1: Paper V, p. 13. Katarina Tunón's 1999 NTNU PhD Thesis "Gestational age in pregnancies conceived after in vitro fertilization, a comparison between age assessed from oocyte retrieval, CRL and BPD" Katarina Tunon, Sturla H. Eik-Nes, Per Gnzmum, Vidar von During, Jarl A. Kahnt, 1999 NTNU PhD Thesis "Ultrasound and Prediction of Gestational Age" Norwegian University of Science and Technology (NTNU), National Center for Fetal Medicine, Department of Gynecology and Obstetrics, ISBN 82-519-1260-1, ISSN 0805-7680)
(Source 2: "Gestational age in pregnancies conceived after in vitro fertilization: a comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter" K. TUNON, S.H. EIK-NES, P. GRØTTUM, V. VON DU¨RING and J.A. KAHN. Ultrasound Obstet Gynecol 2000; 15: 41–46,. p. 45) - Before & After Publication: Abstract Conclusion: Tunón et al. 2000 (p. 41)
"Assessment of gestational age from the time of IVF, CRL and BPD in pregnancies conceived after IVF shows equally high agreement between the three methods. This supports the use of ultrasound as a reliable method for estimation of gestational age." [Note: To be precise, what had been a 1-sentence conclusion was split into 2 sentences, and "in vitro fertilization" was abbreviated to "IVF" for publication.]
- an idea straight out of the Department of the Redundancy Department or
- NCFM Snurra/eSnurra Group believe ultrasound is their must-be-used tool at all times, because...
“To a man with a hammer, everything looks like a nail.” --Mark Twain, or - Conceivably, NCFM Snurra Group did not want to lose the IVFD market else the OTPD market could be next; motivation for changing from a direct GA estimation method to a direct EDD estimation method, which was clearly signaled by their radical conflate-to-obfuscate conclusion change in the "Discussion" section of Tunón et al. 2000, a transition from NCFM Snurra Group's existing GA estimation capability to "estimation of day of delivery ." If only this direct estimation of EDD capability were to have existed in 1999 ... enter Hutchon, 1998 and his 1998 & 1999 manuscript submissions to UOG (because timing is everything for direct EDD estimation), or
- all of the above.
- "The clinical management of the pregnancy was based on gestational age estimated by ultrasound." (Source: Katarina Tunón. 1999 NTNU PhD Thesis. p. 35. "Ultrasound and Prediction of Gestational Age" Norwegian University of Science and Technology (NTNU), National Center for Fetal Medicine, Department of Gynecology and Obstetrics, ISBN 82-519-1260-1, ISSN 0805-7680)
Again, “To a man with a hammer, everything looks like a nail.” --Mark Twain
Closing the Department of the Redundancy Department with Obvious Biological Knowledge
Bergen Group made the point of using "obvious biological knowledge" to end the dubious practice of using suboptimal, unilateral ultrasound-based pregnancy dating to date assisted fertilization pregnancies.
- "We cannot see that age estimation for pregnancy after assisted fertilization needs to be the subject of discussion since we know the time of conception. Still, in many Norwegian hospitals, a correction of the gestational age for these is performed at routine ultrasound, contrary to obvious biological knowledge."
"Vi kan ikke se at aldersbestemmelsen for svangerskap etter assistert befruktning behøver å være gjenstand for diskusjon siden vi vet tidspunktet for befruktning. Fremdeles utføres på mange norske sykehus en korreksjon av svangerskapsalderen hos disse ved rutine ultralyd, stikk i strid med innlysende biologisk kunnskap."
(Source: "Ikke tillitvekkende fra Helsedirektoratet" Dagens Medisin Published: 2014-12-01 12.29, Posted by: Ebbing, Lian Johnsen, Kessler, Kiserud, Everyone at the Women's Clinic, Haukeland University Hospital)
In his seminal article, Bergh 1992, in Tidsskrift for den Norske legeforening, Dr. Johan Bergh reported on 31 perinatal deaths (7.7% in 1991), a notable increase from the prior year (4.2% in 1990) at Rogaland Hospital in Stavanger, Norway. All 31 perinatal deaths had their EDD, which had been established using Naegele's rule, postponed by ultrasound. One of the deaths Dr. Bergh reported resulted after a woman who had become pregnant via in vitro fertilization (IVF) had her factual IVFD-based EDD postponed by 22 days with an NCFM Snurra BPD-based GA from which the woman's EDD had been calculated using Naegele's rule. This was done in accordance with Directorate of Health's 'TUL' policy with their protocol of evidence-obviated medicine. Think about this. A woman's factual in vitro fertilization date (IVFD), the actual definition of GA, had been obviated from all medical evidence to ensure NCFM Snurra Group "estimated" the woman's GA using ultrasound via NCFM Snurra Group's BPD-based GA model and, therefrom, calculate an EDD using Naegele's rule. Again, and to be absolutely clear, the woman's GA did not need to be estimated by ultrasound, as it had already been established, exactly, via in vitro fertilization and her IVFD. Again, IVFD is the definition of GA; it is the 'gold standard' of GA which is used as the reference standard in clinical studies to compare fetal biometry prediction/estimation methods. The 'TUL' policy and protocol of evidence-obviated medicine caused the grossly inaccurate NCFM Snurra BPD-based GA & EDD to be used, which created sub-optimal obstetric and fetal awareness; which caused sub-optimal obstetric and fetal management, which caused increased medical risks, critical medical mistakes and grievous medical harms; risks, mistakes & harms which included perinatal death. Which begs the obvious question: Since the inception of 'TUL' how many times has this happened and, how many times has this resulted in perinatal death? Included below is an excerpt from Bergh 1992.
- "Of the 33 perinatal deaths at the Central Hospital in Rogaland in 1991, seven children were strongly growth-impaired (<3 percentile) compared to the ultrasound period. Five were moderately growth-impaired (3-10 percentile), while the others were not sure of growth retardation. For the three groups, the term after ultrasound was respectively 18, 8 and 5 days later than the term from Naegel's rule. In one case of pregnancy following in vitro fertilization, the ultrasound term was calculated 22 days later than the term on the basis of known time of conception, relative to an ultrasound term set in 18-19 weeks, this can cause serious consequences in early growth retardation. Earlier ultrasound testing will provide more reliable term provision. The malformation diagnosis should be separate from the term provision."
- "The value of an objective and accurate determination of fetal term is indisputable. Without a reasonably accurate term, we will not be able to effectively capture the growth-retarded fetuses and follow their growth and development. The earlier the growth retardation, and the more serious it is, the more important it is to know the exact term. It would be paradoxically if the most endangered fetuses get a delayed term by using our great technology. Then a serious growth retardation will be discovered later and often too late. Furthermore, the severity of the growth retardation will be underestimated. We monitor a serious growth-retarded fetus completely differently in 27-28. week than we do 25-26. week and it is a fact that most will manage well when redeemed in the 28th week even though they are small."
("Verdien av en objektiv og sikker fastsettelse av fødselstermin er udiskutabel. Uten en rimelig sikker termin vil vi ikke effektivt være i stand til å fange opp de vekstretarderte fostre og følge deres tilvekst og utvikling. Jo tidligere vekstretardasjonen Opptrer, og jo mer alvorlig den er, desto viktigere er det å kjenne den eksakte terminen. Det vil være paradoksalt hvis de aller mest truede fostre får en forsinket termin ved hjelp av vår flotte teknologi. Da vil en alvorlig vekstretardasjon bli oppdaget senere og ofte for sent. Videre vil alvorlighetsgraden av vekstretardasjonen bli undervurdert. Vi overvåker et alvorlig vekstretardert foster helt annerledes i 27.-28. uke enn vi gjøri 25. -26. uke, og det er et faktum at de fleste vil klare seg bra ved forløsning i 28. uke selv om de er små.") (Source: "Bør ultralydundersøkelsen gjøres tidligere i svangerskapet?" ("Should ultrasound examination be performed earlier in pregnancy?") Bergh, J. (1992). Tidsskrift for den Norske lægeforening : tidsskrift for praktisk medicin, ny række. 1992; 112. 3450-1.)
It appears clear Ministry of Health and Care Services, Directorate of Health and NCFM Snurra Group believed women of IVF pregnancies (and their doctors and midwives) were somehow mathematically challenged and needed an NCFM Snurra BPD-based GA in order to help women of IVF pregnancies (and their doctors and midwives) add 266 (or 268) days to their IVFD or add 280 (or 282) days to their virtual LMPD. Included below is the: 1) calculation from NCFM Snurra BPD-based GA for EDD and 2) calculation from IVFD for EDD. Color text was used to highlight the corresponding similarities and differences between these simple calculations. [Note: Has your head recovered?]
- NCFM Snurra BPD-based GA Calculation for EDD (ultrasound dating required)
NCFM Snurra BPD-based GA was subtracted from the ultrasound date to calculate a virtual LMPD to which 280 (or 282) days were added to calculate EDD.
IVFD Calculation for EDD (ultrasound dating not required)
14 days were subtracted from IVFD to calculate a virtual LMPD to which 280 (or 282) days were added to calculate EDD. Or, more simply, just add 266 (or 268) days to IVFD to calculate EDD.
(Note: LMPD = last menstrual period date; IVFD = in vitro fertilization date; 14 days = 2w+0 = IVFD gestational age (GA); 280 (or 282) days = fixed pregnancy gestation period)
- “To a man with a hammer, everything looks like a nail.” --Mark Twain
- "Gestational age according to CRL was calculated by the equation
t = 35.72 + 1.082L^(1/2) + 1.472L - 0.09749L^(3/2)
developed by Wisser (Wisser et al., 1994) where L is the greatest embryonic length and in practice correlated to the CRL."
Nevertheless, somehow Tunón et al. 2000 found its way (or was guided) through the referees' and editors' reviews and then published in Ultrasound in Obstetrics & Gynecology (UOG) also know as The White Journal, the official journal of the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) of which Sturla H. Eik-Nes was President (1998-2002) at the time, as well as Principal Supervisor of Tunón's 1999 NTNU PhD Thesis and a Tunón et al. 2000 coauthor. Moreover, and again, Tunón et al. 2000 was published with 2 entirely different conclusions, the Abstract conclusion and the Discussion section conclusion, neither of which was supported by the study's data. Moreover, the Discussion section conclusion conflated NCFM Snurra Group's ability to estimate gestational age and NCFM Snurra Group's then nonexistent capability to estimate day/date of delivery (EDD) i.e., via the Hutchon Method of Population-based Direct EDD Estimation (PDEE) (Hutchon, 1998). The reason the capability was non-existent is because NCFM Snurra/eSnurra Group had not appropriated, plagiarized and misused the Hutchon Method of PDEE until later. And, at the same time, 1999, Dr. Hutchon had submitted a more robust manuscript of the Hutchon Method of PDEE to Ultrasound in Obstetrics & Gynecology (UOG), received by UOG 13.07.1999 and coded as UOG 99/155.
Ironically, NCFM Snurra Group's Tunón et al. 2000 is among the 4 cited references "(11-14)" in the excerpt below, taken from page 2 of: COMMITTEE OPINION Number 700, described in the source reference below.
- "Up to and including 13 6/7 weeks of gestation, gestational age assessment based on measurement of the crown-rump length (CRL) has an accuracy of +/- 5-7 days (11-14)." (Source: COMMITTEE OPINION Number 700, May 2017 p.2. Consensus opinion of: 1) The American College of Obstetricians and Gynecologists (ACOG), 2) American Institute of Ultrasound in Medicine (aium) & 3) Society for Maternal · Fetal Medicine)
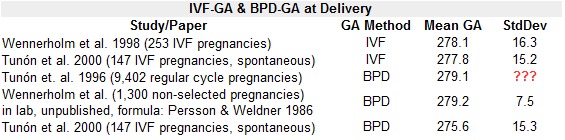
Regarding standard deviation (SD), Tunón et al. 2000 stated:
- "However, in the individual embryo/fetus the difference between the gestational age estimated by IVF and BPD could be as much as 14 days; this has been observed both in the present and a previous study 9."
- "In a non-selected population of 1300 women the mean GA at delivery according to BPD was 279.2 days (SD 7.5) which is the same as the result obtained by Tunón and co-workers in another Nordic population of 15 000 women 3. It is therefore unlikely that this difference in GA is caused by measurement errors." (Source: "Gestational age in pregnancies after in vitro fertilization: comparison between ultrasound measurements and actual age" Wennerholm, C. Bergh, H. Hagberg, B. Sultan and M. Wennergren. Ultrasound Obstet Gynecol 1998;12:170–174. p. 173) Note: Citation 3 was Tunon et al. 1996.
- "The distribution curve of gestational age at delivery according to any method is influenced by preterm births. Due to the negative skewness of the distribution curve of births it is not correct to use parametric statistics such as the mean and the standard deviation to derive the 'true' length of pregnancy. The median and the mode are the more robust estimates."
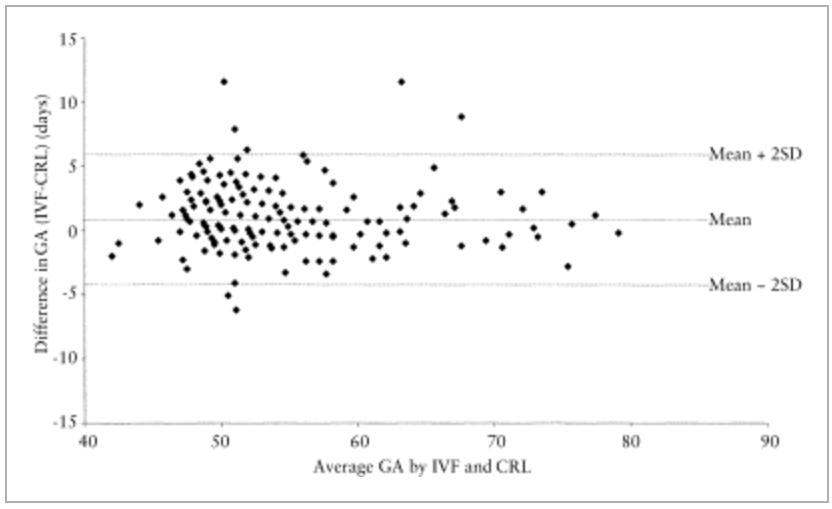
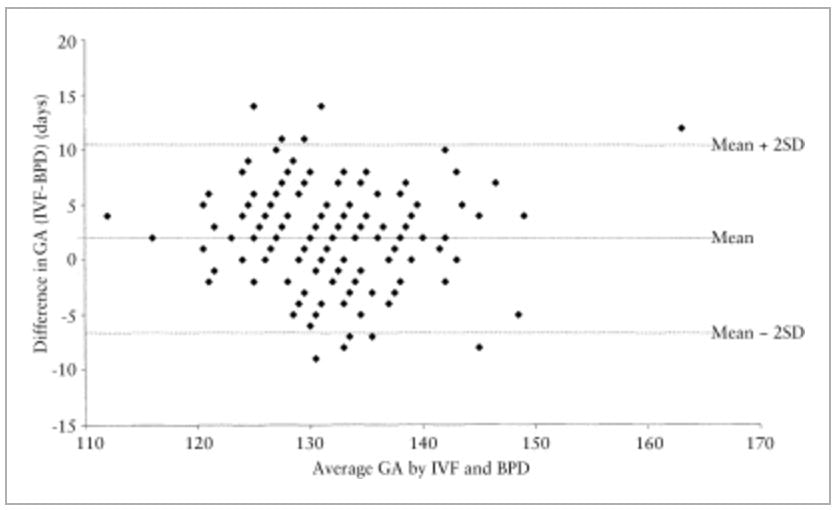
Consider this: Just as SD from Tables 1 & 2 of Tunón et al. 2000 were never discussed, the exact same is true for Figures 1 & 2, of of Tunón et al. 2000, Bland-Altman plots/analyses of 1st-trimester GA: CRL v. IVF and 2nd-trimester GA: BPD v. IVF, respectively. Figures 1 & 2 (included below) were never discussed in Tunón et al. 2000, not once; they just existed, the same as SD simply existed in Tables 1 & 2, respectively. Figures 1 & 2 were begging to be discussed. For example, why was the x-axis of Figure 1 an average of IVF-based GA & CRL-based GA and the x-axis of Figure 2 an average of IVF-based GA & BPD-based GA when the true or actual GA was known, i.e., IVF-based GA? The excerpt below is the one and only mention of Figures 1 & 2, a mere statement of existence. What is strange is, with respect to the Bland-Altman plots/analysis there is no answer to the ubiquitous question of: So what?
- "More detailed analyses are shown in Figures 1 and 2 where the pairwise differences between two measurement techniques are plotted against the average of the measurements 14." (Source: "Gestational age in pregnancies conceived after in vitro fertilization: a comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter" K. TUNON, S.H. EIK-NES, P. GRØTTUM, V. VON DU¨RING and J.A. KAHN. Ultrasound Obstet Gynecol 2000; 15: 41–46,. p. 42-43)
|
Figure 1.
Difference in mean for gestational age assessed by IVF and CRL in singletons (n = 208). GA = gestational age; IVF = in vitro fertilization; CRL = crown–rump length. |
Figure 2.
Difference in mean for gestational age assessed by IVF and BPD in singletons (n = 208). GA = gestational age; IVF = in vitro fertilization; BPD = biparietal diameter. |
No matter how one interprets Figures 1 & 2 (above) these do not substantiate the Tunón et al. 2000 conclusion included below.
- "...the high agreement between the gestational age calculated from the time of IVF and from the early CRL measurements in the same pregnancies, the high agreement between gestational age calculated from the time of IVF and BPD supports the use of ultrasound as a reliable method for estimation of day of delivery both in normally conceived pregnancies and IVF pregnancies."
eeeeeee
"TUL" & IVF
It is difficult to get one's head around the fact Tunón et al. 2000 made it past peer review, UOG referees and was published. And, then, according to Økland's 2012 NTNU dr.philos. Thesis, Tunón et al. 2000 was used to establish the government-mandated protocol of evidence-obviated medicine known as "TUL" (i.e., Term according to Ultrasound (UltraLyd) which, until very recently, required ultrasound dating of all in vitro fertilization pregnancies in Norway. It was unlikely, even before the ubiquity of smartphones with date calculating calendars, a woman would forget or not have a record of her in vitro fertilization date (IVFD). Although, it must be recognized that without a smartphone's built-in date calculator, the addition of 266 days (or 268 days) to a woman's IVFD would have then necessitated other means of calculation. Fortunately, Norway's women are known, intentionally, to be well educated, resourceful problem-solvers; therefore, Directorate of Health decided all women of IVF pregnancies in Norway needed an ultrasound-based NCFM Snurra BPD-based GA (i.e., an estimate of their factual IVFD) and, therefrom, a calculated EDD (i.e., adding 266 days (or 268 days) to IVFD) using the equivalent of Naegele's rule, while unnecessarily exposing women of IVF pregnancies to the known risks inherent in an NCFM Snurra BPD-based GA prediction error and, later, an NCFM eSnurra BPD-based EDD prediction error of which 12.8% are known to be grossly inaccurate (i.e., < -14 or more days or > +14 or more days). And, to think Tunón et al. 2000, according to Økland's 2012 NTNU dr.philos. Thesis, was academic justification for Norway's "TUL" policy of evidence-obviated medicine.
Interestingly and ironically, Tunón et al. 2000 is the 2nd citation "[2]" for Wikipedia's entry: Gestational age for how to ... wait for it ... calculate gestational age for IVF pregnancies, no kidding, as it would be difficult to make this up. The content from the "Methods" section of the Wikipedia entry is included below, followed by the reference. Again, here is the link to the Wikipedia entry: Gestational age, as this should be seen for oneself.
- " • In case of in vitro fertilization, calculating days since oocyte retrieval or co-incubation and adding 14 days.[2]" While the irony alone is confirming, there is more. The citation and reference of Tunón et al. 2000 in Wikipedia serve to confirm the peer review and publication vetting processes of Ultrasound in Obstetrics & Gynecology were on par with the present-day vetting processes of Wikipedia. (Source: Wikipedia: Gestational age)
- References
"2. Tunon, K.; Eik-Nes, S. H.; Grøttum, P.; Von Düring, V.; Kahn, J. A. (2000). "Gestational age in pregnancies conceived after in vitro fertilization: A comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter". Ultrasound in Obstetrics and Gynecology. 15 (1): 41–46. PMID 10776011. doi:10.1046/j.1469-0705.2000.00004.x." (Source: ibid.) - Final point on this ironic tangent: Maybe a credit for Wisser et al. 1994 should be included, as it was their greatest-embryonic-length (GEL) model/equation which had been used, inappropriately and dubiously, by NCFM Snurra Group to estimate "crown-rump length" (CRL) in Tunón et al. 2000.
The spurious conclusions of Tunón et al. 2000, were parroted 7 years later in a Runa Heimstad's 2007 NTNU PhD Thesis. Interestingly, Sturla Eik-Nes, a coauthor of Tunón et al. 2000, was Runa Heimstad's PhD co-supervisor and coauthor of 2 of the 4 papers included within Heimstad's PhD Dissertation.
- "Ultrasound is also found to be a reliable method in pregnancies conceived with assisted reproductive techniques, and assessment of gestational age from the time of IVF, CRL and BPD showed equally high agreement between the three methods. 20" (p. 13) (Source: "Post-term pregnancy" (p. 13). Runa Heimstad. 2007 NTNU PhD Dissertation, Faculty of Medicine, Department of Laboratory Medicine, Children's and Women's Health. ISBN 978-82-471-5398-7 (printed ver.), ISBN 978-82-471-5403-8 (electronic ver.) [Note: Citation 20: "20 Tunón K, Eik-Nes SH, Grøttum P, Von Düring V, Kahn JA. Gestational age in pregnancies conceived after in vitro fertilization: a comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter. Ultrasound Obstet Gynecol 2000;15(1):41-6"]
- "The data that were collected from fetal examinations in Trondheim were used by EikNes et al. to introduce the phrase ‘TUL‘ — Term according to ULtrasound — which for 25 years has been a fixed Norwegian term, resulting in a uniform dating system from ultrasound, regardless of whether the LMP was reliable or not." (Source: Økland 2012 NTNU dr.philos. Thesis, p. 21)
- "In Katarina Tunón's thesis from 1999, 5 studies on different aspects of ultrasound-based pregnancy dating were included (Tunón et al. 1996, Tunón et al. 1998, Tunón et al. 1999b, Tunón et al. 1999a, Tunón et al. 2000), and Snurra was the dating method that was used as the ultrasound-based term prediction model in all the studies. Tunón et al. were able to prove that ultrasound dating should be the method of choice even when LMP-data were reliable (Tunón et al. 1996), and in pregnancies conceived after in vitro fertilization (Tunón et al. 2000)." (Source: Økland 2012 NTNU dr.philos. Thesis, p. 22)
Cue the refrain: To a man with a hammer, everything looks like a nail.” --Mark Twain
- BPD: Loughna et al.
- "Ultrasound societies such as ISUOG (International Society of Ultrasound in Obstetrics and Gynecology) (Salomon et al. 2011), and BMUS (British Medical Ultrasound Society) (Loughna et al. 2009) have published practice guidelines for assessment of fetal size and dating, where structures recommended to be measured and the technique describing how to measure them, are specified." (Source: Økland 2012 NTNU thesis, p. 39)
- "The equation is BPD plus OFD multiplied with a factor of π/2 (1.57) according to the BMUS (Loughna et al. 2009), or 1.62 according to the ISUOG guidelines (Salomon et al. 2011)." (Source: Økland 2012 NTNU dr.philos. Thesis, p. 50)
- "In view of the inaccuracies that may result from using the BPD measurement, the BMUS Fetal Measurements Working Party was of the opinion that the BPD should not be used in routine clinical practice for the estimation of gestational age or the appropriateness of fetal size in later pregnancy. Charts and tables for BPD measurements are therefore not presented in this document." (Source: ULTRASOUND, August 2009, Volume 17, Number 3, "Fetal size and dating: charts recommended for clinical obstetric practice" Pam Loughna1 , Lyn Chitty2 , Tony Evans3 & Trish Chudleigh4, 1 Academic Division of Obstetrics and Gynaecology, Nottingham University Hospitals NHS Trust, 2 Genetics and Fetal Medicine, Institute of Child Health and University College London Hospitals NHS foundation Trust, London, 3 Medical Physics, University of Leeds, Leeds and 4 The Rosie Hospital, Cambridge, UK)
- "The Directorate of Health also ignores published criticism of the Trondheim study (4): selection bias before and after weeks 18 – 20 of gestation; unclear exclusion criteria for fetuses with potentially hampered growth; and failing to account for the inclusion of fetuses with an elongated head whose biparietal diameter was adjusted based on the longitudinal axis of the skull." (Source: "Flawed recommendation issued by the Norwegian Directorate of Health concerning the determination of fetal age", Nr. 8, 5 mai 2015, Tidsskr Nor Legeforen, 2015; 135:7401, DOI: 10.4045/tidsskr.15.0093) Reference (4): (Source: Re: A direct method for ultrasound prediction of day of delivery:a new, population-based approach. Problems of accounting for a retrospective selection. Kiserud T, Johnsen SL, Rasmussen S., Ultrasound Obstet Gynecol 2008; 31: 22)
- "The BPD measurement is dependent on head shape (which, to some extent, can be quantified using the cephalic index), whilst the head circumference measurement is independent of head shape. Therefore for fetuses with a dolicocephalic head shape, the head circumference will be within expected limits, but the BPD recorded will be smaller than the normal value for a given GA. If the BPD measurement is used to date such pregnancies, they will incorrectly be assigned a gestational age which is less than that expected from the last menstrual period (LMP) or the head circumference measurement. This effect of using the BPD for dating pregnancies has been reported by two groups (Hadlock et al., 1 Altman and Chitty, 2)" (Source: "Fetal size and dating: charts recommended for clinical obstetric practice" Pam Loughna, Lyn Chitty , Tony Evans & Trish Chudleigh. ULTRASOUND N August 2009 N Volume 17 N Number 3,, p. 161. References: 1. Hadlock FP, Deter RL, Carpenter RJ, Park SK. Estimating fetal age: effect of head shape on BPD. Am J Roentgenol 1981;137:83–85. 2. Altman DG, Chitty LS. New charts for ultrasound dating of pregnancy. Ultrasound Obstet Gynecol 1997;10:174–191.)
- "The measurements of choice for the estimation of fetal size are shown in Table 2 below. As with dating, because of the potential inaccuracies with the BPD measurement, it is recommended that the head circumference is used to evaluate fetal head size rather than the BPD. For all parameters given below, a single measurement should be used, provided it is of good technical quality and obtained using the techniques and planes described." (Source: ibid., p. 163)
Table 2. Measurements for estimation of fetal size.
Measurement Gestational age range
Head circumference (HC) 13 to 42 completed weeks
Abdominal circumference (AC) 13 to 42 competed weeks
Femur length (FL) 13 to 42 competed weeks
BPD: Salomon et al.
Økland also intentionally ignored the important, highly relevant BPD guideline stated in Salomon et al. 2011 (p. 7): "Age estimates from head sizes (BPD and/or HC) should be used..." It is important to be clear that "(BPD and/or HC)" means do not use BPD alone, use either (BPD & HC) or (HC) for "age estimates from head sizes." Moreover, this guidance was not limited to cases of abnormal fetal head shape.
- "Age estimates from head sizes (BPD and/or HC) should be used if first trimester scan are not available and the menstrual history is unreliable as a result of uncertain dates or irregular periods (17, 18)." (Source: "Practice guidelines for performance of the routinemid-trimester fetal ultrasound scan" L. J. SALOMON, Z. ALFIREVIC, V. BERGHELLA, C. BILARDO, E. HERNANDEZ-ANDRADE,S. L. JOHNSEN, K. KALACHE, K.-Y. LEUNG, G. MALINGER, H. MUNOZ, F. PREFUMO, A. TOIand W. LEE on behalf of the ISUOG Clinical Standards Committee. Ultrasound Obstet Gynecol 2011; 37: 116–126 Published online 7 December 2010 DOI: 10.1002/uog.8831, p. 118, p. 118-119)
- "Abnormal head shape (e.g. brachycephaly and dolichocephaly) can be associated with syndromes. This finding can also lead to inaccurate estimates of fetal age when the BPD is used; in these cases, HC measurements are more reliable 20." p. 118-119 (Source: ibid.)
- "A well-known drawback of the BPD measurement is that it may be influenced by an unusual fetal head shape — a ‘problem‘ detected more often in the third than in the second trimester, and therefore having more consequences for growth assessment than for dating." (Source: Økland 2012 NTNU dr.philos. Thesis, p. 49)
Again, Loughna et al. 2009 and Salomon et al. 2011 made it clear BPD is problematic and unreliable and that HC is a more robust fetal head metric for determining GA during routine ultrasound exams. However, this clear, consistent message, from 2 papers which were cited extensively in Økland's 2012 NTNU dr.philos. Thesis, was intentionally excluded by Økland in the BPD section of her thesis (p. 48-50). The table below shows the number of citations and references to Salomon and Loughna. Note: Gjessing and Tunón are/were NCFM eSnurra and Snurra Group members, respectively.
- Citations by Name (not publication)
Rank Name Citations Cumulative Cum. % of Total
1 Gjessing 41 41 16%
2 Salomon 26 67 26%
3 Tunón 25 92 36%
4 Verburg 19 111 44%
5 Loughna 13 124 49%
(Source: Økland 2012 NTNU TThesis)
Nevertheless, this important, highly relevant fact and issue were actively ignored by Økland and her thesis supervisors because it was inconvenient to the NCFM eSnurra Group's agenda and ambitions. More specifically, HC was not (and is not) an independent variable contained within NCFM eSnurra Group's historical records datasets; the datasets which serve as the foundation upon which the NCFM eSnurra Group's eSnurra "method" was, and is, based. NCFM eSnurra Group cannot sell what it does not have, and they do not have HC-based GA & EDD; ergo, they must promote and sell what they do have, BPD-based EDD & GA, all day, every day, which explains Økland's inordinate interest in HC equations that can be used with cephalic index to calculate an 'adjusted' or 'corrected' BPD instead of including the fact BPD is problematic and unreliable and HC is a more robust predictor of GA during routing ultrasound exams. Again, this speaks loudly, clearly and directly to the ethos of scholarship, academic integrity and independence of Økland, her 2012 NTNU dr.philos. Thesis, her coauthors, her thesis supervisors and her this Assessment Committee members.
- "The long axis might be used to calculate a ‘corrected’ BPD (Kurtz and Goldberg 1988), but if the normality of one dating parameter is doubted, another should be chosen (Degani 2001, Kurtz and Goldberg 1988), and the FL then seems to be a reliable alternative (Geirsson 1991, Gjessing et al. 2007)." (Source: Økland's 2012 NTNU dr.philos. Thesis , p. 49).
Finally, and despite what Loughna et al. 2009, Salomon et al. 2011 and others had stated, Økland concludes the exact opposite in the excerpt below, citing fellow NCFM eSnurra Group's Gjessing et al. 2007 (i.e., which appropriated and plagiarized the Hutchon Method of PDEE).
- "In second-trimester dating, the BPD seems to remain the measurement of choice (Saltvedt et al. 2004), also in newer dating models (Verburg et al. 2008b, Gjessing et al. 2007), and there are probably no systematic differences in EDD predictions from BPD or HC with examinations up to week 20." (Source: Økland's 2012 NTNU dr.philos. Thesis, p. 51)
In the excerpt below, Økland cited Verburg et al. 2008b for the mere fact Verburg used BPD in his study. What Økland does not include is that Verburg also used HC and and did not state a preference for either BPD or HC, but he did state there is controversy over which metric to use and when to measure. However, Vergurg et al. did conclude the earlier (10-12 weeks) the ultrasound assessment, the better the GA estimate (excerpts below). This, highly relevant fact and issue were excluded by Økland because it was inconvenient to the NCFM eSnurra Groups agenda for BPD in second-trimester, routine 18wUSE. This speaks loudly, clearly and directly to the ethos of scholarship, academic integrity and independence of Økland, her 2012 NTNU dr.philos. Thesis, her coauthors and her thesis supervisors.
- "Controversy remains about the measurement of choice and the optimal gestational age for assessment 11." (Source: "New charts for ultrasound dating of pregnancy and assessment of fetal growth: longitudinal data from a population-based cohort study" B. O. Verburg, E. A. P. Steegers, M. De Ridder, R. J. M. Snijders, E. Smith, A. Hofman, H. A. Moll, V. W. V. Jaddoe, J. C. M. Witteman. Ultrasound in Obsterics & Gynecology Volume 31, Issue 4 April 2008. Pages 388–396 First published: 17 March 2008. DOI: 10.1002/uog.5225")
- "Conclusions
Charts for ultrasound dating of pregnancy and reference curves for fetal biometry are presented. The results indicate that, up to 24 weeks of pregnancy, dating by ultrasound examination provides a better prediction of the date of delivery than does last menstrual period. The earlier the ultrasound assessment in pregnancy, preferably between 10 and 12 weeks, the better the estimate of gestational age." (Source: Ibid.) - "It has been established that embryos follow the same growth pattern in early pregnancy 6. Therefore, more accurate information on gestational age can be provided by ultrasound assessment and this is widely recognized to be the method of choice 7, 8. Ultrasound dating of pregnancy is usually based on crown–rump length (CRL) or biparietal diameter (BPD) 9, 10. Controversy remains about the measurement of choice and the optimal gestational age for assessment 11." (Source: ibid.)
- "In clinical practice, substantial differences between gestational age based on ultrasound measurements and LMP, if reliable, should be considered as an indicator of possible pathology and an increased risk of fetal growth restriction 27." (Source: ibid.)
Økland injected FUD into her discussion of HC for determining GA in the "HC" section of her 2012 NTNU dr.philos. Thesis while intentionally ignoring the important, highly relevant facts and issues presented in Loughna et al. 2009 and Salomon et al. 2011 about BPD being problematic and unreliable, as discussed in their charts and practice guidelines. These were inconvenient facts for NCFM eSnurra Group's agenda and ambitions.
- Fear: "Effectively, the HC depends on 2 diameters where the long axis, the OFD, is measured in the lateral direction and is thus vulnerable to the inferior lateral resolution — and may over time be affected by the beam width factor." (p. 51)
- Uncertainty:
1) "There have been discussions on what this measurement [HC] really adds to the accuracy of the assessment of fetal age and growth if the fetal head shape is normal (Gjessing and Grøttum 2007)." (p. 50)
2) "...there are probably no systematic differences in EDD predictions from BPD or HC..."
3) "Dating examinations in the third-trimester are obsolete...but HC measurements are often included in fetal growth formulae for use in third-trimester."
4) "The mathematical problem is that the HC does not represent the circumference of a true ellipse, as the fetal head is rounded posteriorly..." - Doubt: "The way we traditionally measure the HC certainly does not make it independent of the head shape."
- "In view of the inaccuracies that may result from using the BPD measurement, the BMUS Fetal Measurements Working Party was of the opinion that the BPD should not be used in routine clinical practice for the estimation of gestational age or the appropriateness of fetal size in later pregnancy. Charts and tables for BPD measurements are therefore not presented in this document." (Source: ULTRASOUND N August 2009 N Volume 17 N Number 3, p. 161. "Fetal size and dating: charts recommended for clinical obstetric practice" Pam Loughna1 , Lyn Chitty2 , Tony Evans3 & Trish Chudleigh4, 1 Academic Division of Obstetrics and Gynaecology, Nottingham University Hospitals NHS Trust, 2 Genetics and Fetal Medicine, Institute of Child Health and University College London Hospitals NHS foundation Trust, London, 3 Medical Physics, University of Leeds, Leeds and 4 The Rosie Hospital, Cambridge, UK)
- "Dating measurements are used to confirm the postmenstrual dates (if known) or to estimate the gestational age (GA) of the fetus when the menstrual history is unknown or unreliable. Normally the earliest technically satisfactory measurement will be the most accurate for dating purposes. Once the gestational age has been assigned, later measurements should be used to assess fetal size and should not normally be used to reassign gestational age." (Source: ULTRASOUND N August 2009 N Volume 17 N Number 3, p. 161. "Fetal size and dating: charts recommended for clinical obstetric practice" Pam Loughna 1 , Lyn Chitty 2 , Tony Evans 3 & Trish Chudleigh 4, 1 Academic Division of Obstetrics and Gynaecology, Nottingham University Hospitals NHS Trust, 2 Genetics and Fetal Medicine, Institute of Child Health and University College London Hospitals NHS foundation Trust, London, 3 Medical Physics, University of Leeds, Leeds and 4 The Rosie Hospital, Cambridge, UK)
Økland Obviates the "strong evidence"
Under the title "Drawbacks and disagreements" (p. 39) of "The ultrasound method" section of Økland's 2012 NTNU dr.philos. Thesis Økland took exception with Loughna et al. 2009 and Salomon et al. 2011; however, she did this without being specific about what is a "drawback" and what is in "disagreement." Moreover, Økland identifies (i.e., more like scapegoats) "clinicians" as needing "strong evidence" to change their minds, without ever stating that for which "clinicians" might change their minds. Incredulously, Økland stated all this while, simultaneously, she intentionally excluded, or obviated, all the "strong evidence" from her 2012 NTNU dr.philos. Thesis. Specifically, Økland obviated the "strong evidence" of:
- BPD is a problematic, unreliable estimator of GA during routine ultrasound exams and the more robust HC should be used instead, or HC should be used in conjunction with BPD, but BPD should not be used alone.
- first-trimester ultrasound estimates of GA are more reliable than second-trimester estimates and
- CRL is a better predictor of GA than BPD
- "Ultrasound societies such as ISUOG (International Society of Ultrasound in Obstetrics and Gynecology) (Salomon et al. 2011), and BMUS (British Medical Ultrasound Society) (Loughna et al. 2009) have published practice guidelines for assessment of fetal size and dating, where structures recommended to be measured and the technique describing how to measure them, are specified. Unfortunately, such guidelines have a tendency to be released many years too late to really be implemented in common practice, because fulfilling these new standards would involve a rejection of the already established, and apparently well-functioning local practices. It takes strong evidence to change clinicians' minds." p. 39
- "NSFM teaches and trains midwives and doctors in ultrasound diagnostics both in Norway and abroad. In cooperation with the Norwegian University in Technology (NTNU), the center develops new procedures and technologies in fetal medicine. The center is a WHO collaborating center for diagnostic ultrasound in obstetrics and gynecology." (Source: NCFM website)
Menstrual Data: LMPD/OTPD/SCID, etc.
Another of the "published practice guidelines for assessment of fetal size and dating" to which Økland took exception without explicitly stating why was the use of menstrual data, namely LMPD, in conjunction with ultrasound. Again, Loughna et al. 2009 stated in the first sentence of the first paragraph in the "General guidance" section:
- "Dating measurements are used to confirm the postmenstrual dates (if known) or to estimate the gestational age (GA) of the fetus when the menstrual history is unknown or unreliable. Normally the earliest technically satisfactory measurement will be the most accurate for dating purposes. Once the gestational age has been assigned, later measurements should be used to assess fetal size and should not normally be used to reassign gestational age." (Source: Loughna et al. 2009, further above, p. 161)
- "If theLMP is used only for scheduling of the dating examination, all questions where the length of gestation influences the answer will relate to the ultrasound-based GA/EDD after the examination is performed." (Source: Økland's 2012 NTNU dr.philos. Thesis, p. 35)
- "It appears evident that the LMP should be used only in the scheduling of the dating scan (Gardosi et al.1997, Bottomley and Bourne 2009)." (Source: Økland's 2012 NTNU dr.philos. Thesis, p. 30)
- "Moreover, at least in Europe, it became common practice to use the EDD determined at the ultrasound examination, no matter how ‘certain’ the reported LMP might be (Taipale and Hiilesmaa 2001, Bottomley and Bourne 2009, Verburg et al. 2008b)." (Source: Økland's 2012 NTNU dr.philos. Thesis, p. 31)
- "The model [NCFM eSnurra] obviates the dependence on last menstrual period found in standard methods for term prediction, and allows an immediate assessment of prediction quality in a population setting." (Source: "A direct method for ultrasound prediction of day of delivery: a new, population-based approach" H. K. GJESSING, P. GRØTTUM and S. H. EIK-NES; Ultrasound Obstet Gynecol 2007: 30: 19–27)
Ultrasound vs. Reliable LMPD: Only a 6% Difference
Økland, again, was being disingenuous regarding the Tunón et al. 1996 and Tunón et al. 2000 studies she cited, as included in the excerpts below.
- "When Tunón et al. (1996) were able to show that ultrasound dating was superior to dating even from reliable LMPs in a large population, they indeed answered many questions on how to use the ultrasound dating methods. In Norway, this study supported the established policy of using the term according to ultrasound, ‘TUL’, independent of the LMP term date." (Source: Økland's 2012 NTNU dr.philos. Thesis, p. 30)
- "Tunón et al. were able to prove that ultrasound dating should be the method of choice even when LMP-data were reliable (Tunón et al. 1996), and in pregnancies conceived after in vitro fertilization (Tunón et al. 2000)., p. 22).
The stated purpose of Tunón et al. 1996 is included below.
- "The purpose of this study was to compare the ultrasonic measurement of the biparietal diameter with the last menstrual period as the basis for estimation of the day of delivery, and to evaluate the precision of these methods as routine procedures." (Source: "A comparison between ultrasound and a reliable last menstrual period as predictors of the day of delivery in 15 000 examinations" Tunón K, Eik-Nes SH and Grøttum P. Ultrasound Obstet Gynecol 1996; 8: 178-185, p. 179)
- "In women with a reliable menstrual history and spontaneous onset of labor, the ultrasound estimate was the significantly better predictor of the day of delivery in 52% of cases, and the last menstrual period estimate was the better predictor in 46% of cases." (Source: "A comparison between ultrasound and a reliable last menstrual period as predictors of the day of delivery in 15 000 examinations" Tunón K, Eik-Nes SH and Grøttum P. Ultrasound Obstet Gynecol 1996; 8: 178-185, p. 178)
- "It is concluded that ultrasound measurement of the biparietal diameter between 15 and 22 weeks of pregnancy is the best method for estimation of the day of delivery and should be used as a routine procedure." (Source: ibid., p. 178)
- "It is in the interests of the obstetricians to estimate a day which is as close as possible to the actual day of delivery, for as many women as possible. We have shown that the variation of the births around the estimated day of delivery is significantly smaller for the ultrasound method than for the last menstrual period method." (Source: ibid., p. 184)
- "For those with discrepancy between the last menstrual period estimate and the ultrasound estimate, the ultrasound estimate was a better predictor of the day of delivery for most of the deliveries." (Source: ibid., p. 184) [Note: this could mean 7,501 vs. 7,499]
- "The ultrasound method for predicting day of delivery can therefore be recommended as the method of choice." (Source: ibid., p. 184)
This 52% to 46% difference used by Tunón et al. 1996 to conclude ultrasound was "the significantly better predictor of day of delivery" and the resulting "TUL" policy is more like having 9 people dining together at a table in a restaurant to whom coffee was served, with 5 people requesting sugar and the other 4 people requesting cream, while the restaurant mandated a strict policy that excluded the use of both cream and sugar in coffee. Consequently, and in accordance with the restaurant's mandated policy, it was decided by the evidence of 5 to 4, sugar to cream, respectively, that:
- sugar was "the significantly better" coffee additive,
- the option of adding cream to one's coffee was summarily obviated and
- all 9 people at the table were required to add sugar to their coffee, whether they wanted sugar or not.
Also, consider the cost of an additional ultrasound exam vs. the cost of using a reliable LMPD (free), or the cost of using a grossly inaccurate ultrasound EDD & GA, unilaterally and erroneously, for all medical thinking, medical decision-making and medical actions when ultrasound-based GA & EDD could have been cross-checked via a simple comparison with a reliable LMPD or a combined, fully corroborating, factual LMPD/OTPD/SCID-based GA & EDD, or just an OTPD-based GA & EDD, at no additional cost. Again, compare this with the cost of not identifying a fetal pathology masked by a grossly inaccurate ultrasound-based GA & EDD in the sequence of: medical thinking > medical decision-making > medical actions, the very same sequence which results in the scheduling of a medical procedure much too late (e.g., turning a baby from breech to vertex for normal deliver before the onset of labor) based, unilaterally, on a grossly inaccurate ultrasound-based GA & EDD. This is where the words "significantly better" make sense because it costs nothing other than some medical thinking (i.e., thinking unencumbered by confirmation bias or doublethink) to use ultrasound evidence in conjunction with all available information, including reliable LMPD or a fully corroborating, factual LMPD/OTPD/SCID, or just a factual OTPD, to determine the best possible GA & EDD to enable better obstetric medicine, better fetal medicine, better obstetric clinical care and better patients' safety. In short, the 52% to 46% may have been a finding or result in Tunón et al. 1996, but the "significantly better" conclusion drawn from this finding or result on a mere 6% difference is both incredulous and dubious. Also, the use of this conclusion to justify the government-mandated protocol of evidence-obviated medicine, i.e., the "TUL" policy, is downright Orwellian. Tunón used the word "significant" or a variant thereof 56 times throughout her 1999 PhD Thesis. One can only wonder if 6% was the threshold trigger for each use of the word "significant." Yet, and according to Økland's 2012 NTNU dr.philos. Thesis, this 52% to 46% conclusion:
- "supported the established policy of using the term according to ultrasound, ‘TUL’, independent of the LMP term date."
- "to prove that ultrasound dating should be the method of choice even when LMP-data were reliable..."
Ovulation Variance & Ovulation Tests
One cannot help but wonder how a combined, fully corroborating factual LMPD/OTPD/SCID-based GA & EDD or just a factual OTPD-based GA & EDD would perform against ultrasound if this same study methodology were repeated today. A reliable LMPD is not equivalent with reliable date of ovulation for establishing the beginning of pregnancy. LMPD does not eliminate ovulation variance (i.e., follicular phase variance) and, by itself, LMPD does not eliminate insemination to conception variance. Ovulation variance is reported to account for up to 50% of total gestational variance in pregnancies. An ovulation test with a +/- 1 day error, depending on how the test is used (i.e., E3G & LH rise or LH peak) can eliminate ovulation variance from being erroneously allocated into a grossly inaccurate ultrasound-based GA & EDD. Moreover, this very point about ovulation test reliability (excerpt below) was made in Katarina Tunón's 1999 NTNU PhD Thesis (p. 18-19). However, and this is important: No subsequent NCFM Group publication has discussed ovulation tests as a means to eliminate ovulation variance and thus mitigate the risk of assigning a grossly inaccurate GA & EDD to to a pregnancy. NCFM eSnurra Group's agenda requires ovulation variance to be in play, otherwise they would lose GA-days from the days-available-for-allocation inventory and would be forced to consider other issues, including SGA and fetal pathology, to understand and explain large discrepancies between ultrasound-based GA and OTPD-based GA, you know, the critical thinking part of medicine required in the practice of evidence-based medicine which considers all available information.
- "It is likely that no more than one day intervenes between ovulation and fertilization (O'Rahilly and MUller, 1987). In a study on 221 women intending to get pregnant it was found that conception occurred only when intercourse took place during a six-day period that ended on the day of ovulation as estimated by hormonal methods (Wilcox et al., 1995). These findings suggest a short survival time for the oocyte, or maybe a change in the cervical mucus post-ovulatory that obstructs the entry of sperm (Wilcox et al., 1995)." The survival time for spermatozoa in vivo in cervical mucus is 5 days after insemination or intercourse, and occasionally up to 7 days (Perloff and Steinberger, 1964 ). Sperm retain the capacity to fertilize human oocytes in vitro for 5 days at room temperature (Cohen et al., 1985). Fertilization, then can apparently take place no later than one day after ovulation but up to 7 days after the time of intercourse. [Ergo known date of ovulation combined with known date of single-coitus insemination provides solid evidence for establishing the beginning of pregnancy and the clinically important gestational age.] (Source: Katrina Tunón's 1999NTNU PhD Thesis "Ultrasound and Prediction of Gestational Age" Norwegian University of Science and Technology (NTNU), National Center for Fetal Medicine, Department of Gynecology and Obstetrics, ISBN 82-519-1260-1, ISSN 0805-7680, p. 18-19).
- "This variation about the mean due to variation in growth velocities and measurement errors (Persson et al., 1978a) is less than the variations in the follicular phase (Saito et al., 1972; Boyse et at., 1976; Mcintosh et al., 1980; Walker et al., 1988)." (Source: ibid., p. 24)
- It has been shown that CRL dating curves based on the last menstrual period underestimate the gestational age compared to dating curves based on known ovulation date 15. (Source: Paper V (p. 11) in Katrina Tunón 1999 PhD Thesis "Ultrasound and Prediction of Gestational Age" Norwegian University of Science and Technology (NTNU), National Center for Fetal Medicine, Department of Gynecology and Obstetrics, ISBN 82-519-1260-1, ISSN 0805-7680, p. 18) 3222) [Note: Citation 15 of Paper V incorrectly references "Gregor" instead of "MacGregor"] Citation 15 is MacGregor et al. 1987.
"Abstract
Inaccuracies in gestational age assignment based on published crown-rump length data were noted in patients with known ovulation dates. In this study, we tested the hypothesis that crown-rump length data derived from pregnancies with known ovulation dates differ from those of menstrually timed pregnancies. Seventy-two previously infertile women with known dates of ovulation had crown-rump length measurements from 35-79 days postovulation. We transformed the data to menstrual age (gestational age) by adding 14 days to the date of ovulation and compared our crown-rump length values with those of two previous reports. At corresponding crown-rump length values, the gestational ages from our data differed from those in the previous studies. We suggest using crown-rump length dating curves based on ovulation-timed pregnancies because crown-rump length data derived from menstrually dated pregnancies underestimate true gestational age." (Source: "Underestimation of gestational age by conventional crown-rump length dating curves." MacGregor SN, Tamura RK, Sabbagha RE, Minogue JP, Gibson ME, Hoffman DI. Obstet Gynecol. 1987 Sep;70(3 Pt 1):344-8.)
NCFM eSnurra Group's models in conjunction with Directorate of Health's government-mandated protocol of evidence-obviated medicine cannot incorporate a factual LMPD/OTPD/SCID because while NCFM eSnurra Group appropriated and plagiarized the Hutchon Method of PDEE, they also misused, and continue to misuse it. All time for a pregnancy begins on the date of the ultrasound exam for the Hutchon Method of PDEE. Ergo, LMPD, OTPD, SCID etc. cannot be entered into the actual NCFM eSnurra model to eliminate ovulation (or follicular phase) variance and other variances. Moreover, Directorate of Health's government-mandated protocol of evidence-obviated medicine mandates unilateral reliance on ultrasound-based data while actively excluding consideration of all available information. And, this is precisely why Dr. Hutchon explicitly stated the following in his seminal Hutchon 1998.
- "The chart is only for estimating the date of delivery. "
- "Just as Boerhaave was not actually measuring the length of pregnancy, and the word "gestation" is used to describe the measurement of time from the last menstrual period to reflect this, so also there is no pretence that this method is determining fetal age."
- "The approach mimics, in modern terms, the method originally formulated by Boerhaave. By adopting this approach we do not need to concern ourselves about the length of the cycle nor the certainty of the dates. Provided the fetus can be assessed as normal using other criteria, this chart can be used to provide the best estimate of the date of delivery (EDD)."
- "The true variability of the BPD in the early second trimester (the range of 2 SD) has been found to correspond to ±5-6 days 16. Where data have been obtained from women with a known date of ovulation 16 or from pregnancies from in vitro fertilization 17, the variation diminishes." (Source: Fetal outcome when the ultrasound estimate of the day of delivery is more than 14 days later than the last menstrual period estimate" K. Tunón, S. H. Eik-Nes and P. Grøttum. Ultrasound Obstet Gynecol 1999;14:17–22, p. 21)
- "It is likely that no more than one day intervenes between ovulation and fertilization (O'Rahilly and MUller, 1987). In a study on 221 women intending to get pregnant it was found that conception occurred only when intercourse took place during a six-day period that ended on the day of ovulation as estimated by hormonal methods (Wilcox et al., 1995). These findings suggest a short survival time for the oocyte, or maybe a change in the cervical mucus post-ovulatory that obstructs the entry of sperm (Wilcox et al., 1995)."
Tunón et al. stated LMP-based EDD had been "corrected for cycle length" (excerpt below); however, no method, nor algorithm, nor formula, nor equation, nor reference was disclosed or cited to define "corrected" in this context. One would think full disclosure and full transparency of the method used to "correct" the data would be important in a study comparing LMP-based EDD with ultrasound-based EDD, which begs the question: Were these LMP-based EDDs "corrected" using a secret formula known only to NCFM Snurra Group? The answer, of course, is yes, because the method was not disclosed. Even if this formula is simple or common, it should have been disclosed.
- "The menstrual cycle was considered regular when the interval was 28 ± 4 days. The estimated day of delivery based on the last menstrual period was corrected for the cycle length."
Fear, Uncertainty and Doubt (FUD) for IVF
In the excerpt below, Økland was spreading fear, uncertainty and doubt (FUD) regarding the us of IVF date for pregnancy dating and fetal growth because using IVF date was not (and is not) on the NCFM eSnurra Group agenda. IVF is highly inconvenient and problematic for NCFM eSnurra Group because:
Økland injects FUD to cast aspersions on IVF-dated pregnancies
FUD-injected Tangent for IVF-based GA
Økland cited Saltvedt et al. 2004 a total of 11 times throughout her 2012 NTNU dr.philos. Thesis. However, Økland ignored the important, highly relevant conclusion of Saltvedt et al. 2004:
More FUD & IVF-based GA
Tunón cited Ertzeid et al. 1993 regarding studies using mice, repeatedly, as a FUD-injected tangent regarding the use of IVF-based GA in pregnancies in the main section of her 1999 NTNU PhD Thesis, twice, and in Tunón et al. Paper V included in her 1999 NTNU PhD Thesis and Tunón et al. 2000 (excerpts below).
Tunón et al. cautioned about "applying such findings [in mice] to humans," directly after she had applied "such findings [in mice] to humans" because, after all, her 1999 PhD Thesis titled "Ultrasound and Prediction of Gestational Age" was a gestational age study of humans, not mice. Moreover, there was no evidence nor results reported in Tunón et al. Paper V to suggest IVF-based GA was anything other than reliable and accurate, i.e., other than the conclusion, of course. Again, this was just another FUD-injected tangent to cast aspersions on IVF-based GA. This speaks loudly, clearly and directly to the ethos of scholarship, academic integrity and independence of Tunón, her 1999 NTNU PhD Thesis, her coauthors and her thesis supervisors.
Also, Tunón reported a finding from Dickey & Gasser 1993 regarding differences in CRL among IVF pregnancies (first excerpt). This was another FUD-injected tangent. Note the use of the words "might not be equal." However, and yet again, what Tunón et al. intentionally excluded was the actual conclusion in Dickey & Gasser 1993 (second excerpt), specifically the third point in the results: "the differences are minimized after day 68," this important, highly relevant result was ignored.
IVF-based GA is Actual GA or the Reference Standard
Given all the FUD-injected tangents by Tunón et al. regarding IVF-based GA it is interesting to note Geirsson & Have 1993 and Wennerholm et al. 1998 both defined IVF-based GA as actual gestational age in the titles of their respective papers (excerpts below) comparing IVF-based GA with BPD- and FL-based GA, and both of these papers were cited in Tunón et al. 2000 a total of 8 and 5 times, respectively. The FUD-injected tangents of Tunón et al. were neither science nor research, but they did speak to NCFM Snurra Group's agenda and to the ethos of scholarship, academic integrity, and independence of Tunón, her 1999 NTNU PhD Thesis, her coauthors, thesis supervisors and her thesis Assessment Committee members.
Concluding FUD for IVF-based GA
Admittedly, it was difficult to find a better (or more humorous) FUD-injected tangent than NCFM Snurra Group's use of the mice from Ertzeid et al. 1993. However, there is one final FUD fact worth noting to conclude FUD for IVF-based GA. The polynomial regression GEL-based GA model equation developed in Wisser et al. 1994; the model equation used by NCFM Snurra Group, inappropriately, in Tunón et al. 2000 to estimate CRL-based GA (i.e., NCFM Snurra Group used a GEL-based GA model to estimate GA for CRL measurements, without explanation) instead of using NCFM Snurra Group's own CRL-based GA model. Given all the FUD-injected tangents by NCFM Snurra Group regarding IVF-based GA in Tunón et al. 2000 it seems more than strange NCFM Snurra Group were not the least bit concerned: 1) the model equation developed in Wisser et al. 1994 was constructed from greatest embryonic length (GEL) measurements (not CRL measurements) and 2) in the construction of the GEL-based GA model equation, GA had been established from IVF-based GA dated embryos from 160 women who had become pregnant by 1 of 3 IVF procedures:
In the excerpt below, Økland was spreading fear, uncertainty and doubt (FUD) regarding the us of IVF date for pregnancy dating and fetal growth because using IVF date was not (and is not) on the NCFM eSnurra Group agenda. IVF is highly inconvenient and problematic for NCFM eSnurra Group because:
- IVF date exists,
- for NCFM eSnurra Group's "method" time does not exists in a pregnancy before the routine 18wUSE. Consequently, NCFM eSnurra models when used within a government-mandated protocol of evidence-obviated medicine cannot incorporate a factual IVFD or a factual OTPD or a factual SCID or a factual LMPD into their GA assessments and assignments
- dating of IVF pregnancies does not require ultrasound assessment of GA, which meant IVF pregnancies did not require NCFM eSnurra Group for ultrasound-based EDD and, therefrom, a calculated GA using the equivalent of Naegele's rule, in reverse.
Økland injects FUD to cast aspersions on IVF-dated pregnancies
- "Reports in later years have caused concern, showing that assisted fertilization is associated with increased risks of adverse outcome (Jackson et al. 2004). Probably, these complications can be attributed to the factors leading to the infertility, rather than to the IVF in itself (Romundstad et al. 2008). Consequently, it has not been confirmed that the IVF pregnancies can reasonably be regarded as representative of normally conceived pregnancies when it comes to assessment of dating or growth (Chalouhi et al. 2011)." (Source Økland NTNU 2012 thesis, p. 41)
- INTERPRETATION: Birthweight, gestational age, and risks of small for gestational age babies, and preterm delivery did not differ among infants of women who had conceived both spontaneously and after assisted fertilisation. The adverse outcomes of assisted fertilisation that we noted compared with those in the general population could therefore be attributable to the factors leading to infertility, rather than to factors related to the reproductive technology. (Source: "Effects of technology or maternal factors on perinatal outcome after assisted fertilisation: a population-based cohort study" Liv Bente Romundstad, MD, Pål R Romundstad, PhD, Prof Arne Sunde, PhD, Vidar von Düring, MD, Prof Rolv Skjærven, PhD, Prof David Gunnell, PhD, Prof Lars J Vatten, MD. The Lancet Volume 372, No. 9640, p737–743, 30 August 2008. DOI: http://dx.doi.org/10.1016/S0140-6736(08)61041-7. Published: 31 July 2008)
FUD-injected Tangent for IVF-based GA
- Fear: IVF is "associated with increased risks of adverse outcomes" (Note: Økland deceptively conflated the fear of "adverse outcomes" with using IVF date for pregnancy "dating or fetal growth," when the issues of "outcomes" and using IVF for "dating or growth" are completely separate issues.
- Uncertainty: IVF "probably" not "associated with increased risks of adverse outcome pregnancies" (Note: Again, "outcomes" is a completely separate issue than using IVF for "dating or growth", but Økland deceptively conflated them to inject fear and uncertainty.
- Doubt: "not been confirmed that the IVF pregnancies can reasonably be regarded as representative of normally conceived pregnancies when it comes to assessment of dating or growth." Økland injected the doubt by intentionally not stating IVF had not been disconfirmed, either. Again, Økland was injecting FUD into the use of IVF to push the NCFM eSnurra Group's agenda.
Økland cited Saltvedt et al. 2004 a total of 11 times throughout her 2012 NTNU dr.philos. Thesis. However, Økland ignored the important, highly relevant conclusion of Saltvedt et al. 2004:
- "Therefore, calculating gestational age from oocyte retrieval in IVF pregnancies is probably the closest we can come to true gestational age." (Source: "Ultrasound dating at 12–14 or 15–20 weeks of gestation? A prospective cross-validation of established dating formulae in a population of in-vitro fertilized pregnancies randomized to early or late dating scan" S. SALTVEDT, H. LMSTROM, M. KUBLICKAS, M. REILLY, L. VALENTIN and C. GRUNEWALD. Ultrasound Obstet Gynecol 2004; 24: 42–50, p. 48. Published online 4 May 2004. DOI: 10.1002/uog.1047)
- "Mean age and the rate of nullipara are usually higher in women who have conceived after IVF than in those who have conceived spontaneously 23,24. However, case control studies comparing IVF pregnancies and naturally conceived pregnancies matched for age, parity, time and location of birth, and number of fetuses have shown very similar obstetric outcome concerning pregnancy duration and maternal and fetal complications 25,26. Therefore, calculating gestational age from oocyte retrieval in IVF pregnancies is probably the closest we can come to true gestational age." (Source: ibid.)
- "In second-trimester dating, the BPD seems to remain the measurement of choice (Saltvedt et al. 2004), also in newer dating models (Verburg et al. 2008b, Gjessing et al. 2007), and there are probably no systematic differences in EDD predictions from BPD or HC with examinations up to week 20." (Source: Økland's 2012 NTNU dr.philos. Thesis p. 51)
- "The aim of the present study was to determine the accuracy of different dating formulae in estimating gestational age when dating was performed at 12–14 and 15–20 weeks. For this purpose, 10 published dating formulae based on BPD or BPD/FL were applied to a population of singleton pregnancies conceived after in-vitro fertilization (IVF)." (Source: "Ultrasound dating at 12–14 or 15–20 weeks of gestation? A prospective cross-validation of established dating formulae in a population of in-vitro fertilized pregnancies randomized to early or late dating scan" S. SALTVEDT, H. LMSTROM, M. KUBLICKAS, M. REILLY, L. VALENTIN and C. GRUNEWALD. Ultrasound Obstet Gynecol 2004; 24: 42–50, p. 48. Published online 4 May 2004. DOI: 10.1002/uog.1047)
- "Therefore, calculating gestational age from oocyte retrieval in IVF pregnancies is probably the closest we can come to true gestational age." (Source: ibid.)
More FUD & IVF-based GA
Tunón cited Ertzeid et al. 1993 regarding studies using mice, repeatedly, as a FUD-injected tangent regarding the use of IVF-based GA in pregnancies in the main section of her 1999 NTNU PhD Thesis, twice, and in Tunón et al. Paper V included in her 1999 NTNU PhD Thesis and Tunón et al. 2000 (excerpts below).
- "Studies in mice have indicated that treatment with gonadotropin as it is used in in-vitro fertilization may have adverse effects such as delayed implantation (Ertzeid et al 1993)." (Source: Katarina Tunón 1999 NTNU PhD Thesis "Ultrasound and Prediction of Gestational Age" p.19, Norwegian University of Science and Technology (NTNU), National Center for Fetal Medicine, Department of Gynecology and Obstetrics, ISBN 82-519-1260-1, ISSN 0805-7680)
- "Studies in mice have indicated that treatment with gonadotropin as it is used in in-vitro fertilization may impair embryonic/fetal development (Ertzeid et al., 1993)." (Source: Katarina Tunón 1999 PhD Thesis "Ultrasound and Prediction of Gestational Age" p. 20, Norwegian University of Science and Technology (NTNU), National Center for Fetal Medicine, Department of Gynecology and Obstetrics, ISBN 82-519-1260-1, ISSN 0805-7680)
- "Studies in mice have indicated that treatment with gonadotropin as it is used in in-vitro fertilization may have adverse effects such as delayed implantation and impaired embryonic/fetal development 18. However, one must be cautious about applying such findings to humans." (Source: Paper V, p. 11, Katarina Tunón 1999 PhD Thesis "Ultrasound and Prediction of Gestational Age" p.19, Norwegian University of Science and Technology (NTNU), National Center for Fetal Medicine, Department of Gynecology and Obstetrics, ISBN 82-519-1260-1, ISSN 0805-7680)
- Studies in mice have indicated that treatment with gonadotropin as it is used in IVF may have adverse effects such as delayed implantation and impaired embryonic/fetal development 19. However, one must be cautious about applying such findings to humans. (Source: "Gestational age in pregnancies conceived after in vitrofertilization: a comparison between age assessed from oocyteretrieval, crown-rump length and biparietal diameter" K. TUNON, S.H. EIK-NES, P. GRØTTUM, V. VON DU¨RING and J.A. KAHN. Ultrasound Obstet Gynecol 2000; 15: 41–46,. p 45)
- "Conclusion: Treatment with gonadotropins impaired implantation and embryonic/fetal development. Changes in maternal milieu, rather than in embryo quality, may be responsible for the adverse effects observed." (Source: "Treatment with gonadotropins impaired implantation and fetal development in mice" G. Ertzeid, R. Storeng, T. Lyberg. Journal of Assisted Reproduction and Genetics, May 1993, Volume 10, Issue 4, pp 286–291, p. 286)
Tunón et al. cautioned about "applying such findings [in mice] to humans," directly after she had applied "such findings [in mice] to humans" because, after all, her 1999 PhD Thesis titled "Ultrasound and Prediction of Gestational Age" was a gestational age study of humans, not mice. Moreover, there was no evidence nor results reported in Tunón et al. Paper V to suggest IVF-based GA was anything other than reliable and accurate, i.e., other than the conclusion, of course. Again, this was just another FUD-injected tangent to cast aspersions on IVF-based GA. This speaks loudly, clearly and directly to the ethos of scholarship, academic integrity and independence of Tunón, her 1999 NTNU PhD Thesis, her coauthors and her thesis supervisors.
Also, Tunón reported a finding from Dickey & Gasser 1993 regarding differences in CRL among IVF pregnancies (first excerpt). This was another FUD-injected tangent. Note the use of the words "might not be equal." However, and yet again, what Tunón et al. intentionally excluded was the actual conclusion in Dickey & Gasser 1993 (second excerpt), specifically the third point in the results: "the differences are minimized after day 68," this important, highly relevant result was ignored.
- "The time span from ovulation to fertilization and implantation in pregnancies conceived in natural cycles might not be equal to that in in vitro fertilized pregnancies. In a study on 107 pregnancies from an assisted fertilization program, differences in the CRL in pregnancies with the same age were found (Dickey and Gasser, 1993)." (Source: "Ultrasound evidence for variability in the size and development of normal human embryos before the tenth post-insemination week after assisted reproductive technologies" Richard P. Dickey Raymond F. Gasser, Hum Reprod (1993) 8 (2): 331-337. p. 331. DOI: https://doi.org/10.1093/oxfordjournals.humrep.a138046)
- "The results suggest firstly that marked differences occur in the rate of early human development, secondly, that the differences occur prior to day 27 when observable cardiac activity begins, and thirdly, that the differences are minimized after day 68 when the embryonic period of development is completed." (Source: ibid.)
IVF-based GA is Actual GA or the Reference Standard
Given all the FUD-injected tangents by Tunón et al. regarding IVF-based GA it is interesting to note Geirsson & Have 1993 and Wennerholm et al. 1998 both defined IVF-based GA as actual gestational age in the titles of their respective papers (excerpts below) comparing IVF-based GA with BPD- and FL-based GA, and both of these papers were cited in Tunón et al. 2000 a total of 8 and 5 times, respectively. The FUD-injected tangents of Tunón et al. were neither science nor research, but they did speak to NCFM Snurra Group's agenda and to the ethos of scholarship, academic integrity, and independence of Tunón, her 1999 NTNU PhD Thesis, her coauthors, thesis supervisors and her thesis Assessment Committee members.
- "Comparison of actual and ultrasound estimated second trimester gestational length in in-vitro fertilized pregnancies" (Source: Geirsson & Have 1993) (Source: "Comparison of actual and ultrasound estimated second trimester gestational length in in-vitro fertilized pregnancies" Reynir T. Geirsson, Grethe Have. AOGS Acta Obsetrica et Gynecologica Scandinavica Volume 72, Issue 5, July 1993, Pages 344–346. First published: July 1993 DOI: 10.3109/00016349309021109)
- "Gestational age in pregnancies after in vitro fertilization: comparison between ultrasound measurements and actual age" (Source: "Gestational age in pregnancies after in vitro fertilization: comparison between ultrasound measurements and actual age" Wennerholm, C. Bergh, H. Hagberg, B. Sultan and M. Wennergren. Ultrasound Obstet Gynecol 1998;12:170–174. p. 173)
Concluding FUD for IVF-based GA
Admittedly, it was difficult to find a better (or more humorous) FUD-injected tangent than NCFM Snurra Group's use of the mice from Ertzeid et al. 1993. However, there is one final FUD fact worth noting to conclude FUD for IVF-based GA. The polynomial regression GEL-based GA model equation developed in Wisser et al. 1994; the model equation used by NCFM Snurra Group, inappropriately, in Tunón et al. 2000 to estimate CRL-based GA (i.e., NCFM Snurra Group used a GEL-based GA model to estimate GA for CRL measurements, without explanation) instead of using NCFM Snurra Group's own CRL-based GA model. Given all the FUD-injected tangents by NCFM Snurra Group regarding IVF-based GA in Tunón et al. 2000 it seems more than strange NCFM Snurra Group were not the least bit concerned: 1) the model equation developed in Wisser et al. 1994 was constructed from greatest embryonic length (GEL) measurements (not CRL measurements) and 2) in the construction of the GEL-based GA model equation, GA had been established from IVF-based GA dated embryos from 160 women who had become pregnant by 1 of 3 IVF procedures:
- IVF embryo transfer, 28 cases
- gamete intrafallopian transfer, 117 cases
- intrauterine insemination, 15 cases
- "The calculated regression gives the most precise estimation of gestational age from a single ultrasound measurement of greatest embryonic length. The precise estimation of gestational age in our study is due to the homogeneity of the study population in terms of gestational age. To our knowledge, no different embryonic growth pattern, depending on the procedure of assisted reproduction, has been described."
GUIDELINE 15:
- "The importance of citing the original observation
Another area of concern is the failure to cite the author who first reports the phenomenon being studied. Apparently, some authors instead cite later studies that better substantiate the original observation. Often, this outcome is a result of our attempts at being concise or perhaps a journal’s limitation on the numbers of references that can be included in an article. Admittedly, some discoveries and their originators are so well-known that they are treated as common knowledge within the immediate domain-specific research community. However, in cases in which the pertinent information may not be generally known, it is important to acknowledge and credit the original discovery. As Zigmond and Fischer (2002) note, failure to cite the original report denies the individual who made the initial discovery his/her due credit." (Source: U.S. Department of Health and Human Services (HHS) Office of Research Integrity (ORI): "Avoiding Plagiarism, Self-plagiarism, and Other Questionable Writing Practices: A Guide to Ethical Writing" "This guide was written by Miguel Roig, PhD, from St. Johns University with funding from ORI. This module was originally created in 2003 and revised in 2006 and 2015." View/Download pdf here.) - "Inappropriate Manipulation of References
In a later section I discuss the tendency on the part of some authors to provide what others view as a biased review of the relevant literature. That is, in placing their data or theory in the context of existing relevant work, authors sometimes cite only references that are favorable to their position. However, consistent with the basic tenets of ethical writing and scientific objectivity, we have a responsibility to cite all relevant material, even work that may contradict our own position. Failure to do so compromises our professional obligation to remain unbiased and is antithetical to the primary mission of a scientist’s search for truth." (Source: ibid.)
"It's déjà vu all over again."
In the process of reading Katarina Tunón's 1999 NTNU PhD Thesis and Inger Økland's 2012 NTNU dr.philos. Thesis in conjunction with their 5 and 4 included papers, respectively, one gets the distinct impression one is reading the same text in the main thesis and in the included papers. A famous quotation generally, but not necessarily correctly attributed to Yogi Berra (famous American professional baseball player, manager & coach) captures the feeling: "It's déjà vu all over again." Consequently, these 2 doctoral theses were investigated via text analyses to identify exact, character-for-character, unique (i.e., no multiples counted) text segment matches between 2 text sources: Source A = the main thesis and Source B = the papers included in the theses, i.e., 5 papers for Tunón's 1999 NTNU PhD Thesis and 4 papers for Økland's 2012 NTNU dr.philos. Thesis. The results of exact, character-for-character, unique text segment matches greater than or equal to 10 words are presented in the graph below. To be absolutely clear, this was a comparison of 2 intra-theses text analyses, not an inter-theses text analysis.
In the process of reading Katarina Tunón's 1999 NTNU PhD Thesis and Inger Økland's 2012 NTNU dr.philos. Thesis in conjunction with their 5 and 4 included papers, respectively, one gets the distinct impression one is reading the same text in the main thesis and in the included papers. A famous quotation generally, but not necessarily correctly attributed to Yogi Berra (famous American professional baseball player, manager & coach) captures the feeling: "It's déjà vu all over again." Consequently, these 2 doctoral theses were investigated via text analyses to identify exact, character-for-character, unique (i.e., no multiples counted) text segment matches between 2 text sources: Source A = the main thesis and Source B = the papers included in the theses, i.e., 5 papers for Tunón's 1999 NTNU PhD Thesis and 4 papers for Økland's 2012 NTNU dr.philos. Thesis. The results of exact, character-for-character, unique text segment matches greater than or equal to 10 words are presented in the graph below. To be absolutely clear, this was a comparison of 2 intra-theses text analyses, not an inter-theses text analysis.
- For example: there were 44 and 40 text segment unique matches (y-axis) for Tunón and Økland, respectively, which contained 20 or more words in their respective exact, unique text segment matches (x-axis).
Unless this graph (above) represents the standard profile for text segments copying in an NTNU doctoral thesis (doubtful), there was something truly interesting going on here, which begs the question: What was common to both Tunón's 1999 NTNU PhD Thesis and Økland's 2012 NTNU dr.philos. Thesis given the otherwise healthy 13-year separation between them? Following is a set of elements common to both Tunón and Økland's NTNU doctoral theses:
- NTNU conferred both degrees: PhD (Tunón, 1999) and dr.philos (Økland, 2012)
- Sturla H. Eik-Nes selected, invited and introduced both Tunón and Økland to medical research
- National Center for Fetal Medicine (NCFM), headed by Sturla H. Eik-Nes, identified and headed the theses' research
- NCFM Snurra & eSnurra Groups: NCFM Snurra Group (Tunón) and NCFM eSnurra Group (Økland)
- Theses topic: Ultrasound-based fetal biometry: GA (Tunón) and EDD (Økland)
- Thesis Principal Supervisor: Sturla H. Eik-Nes
- Thesis Co-supervisor: Per Grøttum
- Sturla H. Eik-Nes and Per Grøttum were coauthors on all the papers, included in both NTNU theses
- Nancy Lea Eik-Nes (spouse of Sturla H. Eik-Nes) revised all the manuscripts, i.e., both NTNU theses and all the papers included therein.
- Ultrasound in Obstetrics & Gynecology, the official journal of ISUOG, of which Sturla H. Eik-Nes was President (1998-2002), published all papers included within Tunón's 1999 NTNU PhD Thesis and Økland's 2012 NTNU dr.philos. Thesis.
Verbatim Text Segments Copying
Included below is just one example among several of the copying of large, verbatim, character-for-character, text segments from the papers included in Økland's thesis into her main thesis. The color-coded text segments in Text Source A are from Økland's main thesis. These color-coded text segments map to corresponding color-coded text segments in Text Source B which are from Paper IV included in Økland's thesis. The black text which separates the color-coded text segments are the minor word switch changes made in Økland's main thesis which served to reduce the word-count in individual text segment matches. The effect of this was to lower the number of high word-count text segment matches while, simultaneously, increasing the number of lower word-count text segment matches. For example, if the minor word switch changes (i.e., the black text) had not been made, there would be only 1 large, 1 color text segment match, i.e., the entire 200-word paragraph, which would be 3X larger than Økland's maximum word-count text segment match of 64 words. [Note: black underlined text is text which was not copied from Paper IV into Økland's main thesis. A black X identifies where a word had been deleted from the text copied into Økland's main thesis, causing the same effect as a word switch change.]
Moreover, Økland's Paper IV had been published by UOG in 2011 as: "Narrowed beam width in newer ultrasound machines shortens measurements in the lateral direction: fetal measurement charts may be obsolete" I. ØKLAND, G. BJASTAD. T. F. JOHANSEN, H. K. GJESSING, P. GRØTTUM and S. H. EIK-NES, Ultrasound Obstet Gynecol 2011; 38: 82–87. DOI: 10.1002/uog.8954. Consequently, ISUOG and/or John Wiley & Sons, Ltd. owned the copyright before Økland's 2012 NTNU dr.philos. Thesis had been publicly defended, so there were copyright issues involved given that Økland did not cite the sources for any of the many text segments she copied, verbatim, into her main thesis from the copyrighted papers included in her thesis. [Note: Paper III in Økland's 2012 NTNU dr.philos. Thesis had been accepted for publication in August 2011, but not published until May 2012, 4 months after Økland's public defense in January 2012. A similar situation existed for Paper V included in Tunón's 1999 NTNU PhD Thesis, which was identified earlier on this page.]
Included below is just one example among several of the copying of large, verbatim, character-for-character, text segments from the papers included in Økland's thesis into her main thesis. The color-coded text segments in Text Source A are from Økland's main thesis. These color-coded text segments map to corresponding color-coded text segments in Text Source B which are from Paper IV included in Økland's thesis. The black text which separates the color-coded text segments are the minor word switch changes made in Økland's main thesis which served to reduce the word-count in individual text segment matches. The effect of this was to lower the number of high word-count text segment matches while, simultaneously, increasing the number of lower word-count text segment matches. For example, if the minor word switch changes (i.e., the black text) had not been made, there would be only 1 large, 1 color text segment match, i.e., the entire 200-word paragraph, which would be 3X larger than Økland's maximum word-count text segment match of 64 words. [Note: black underlined text is text which was not copied from Paper IV into Økland's main thesis. A black X identifies where a word had been deleted from the text copied into Økland's main thesis, causing the same effect as a word switch change.]
- Text Source A: Økland's 2012 NTNU dr.philos Thesis, Statistical methods, Study 4, p. 66
We analyzed the 41 941 FL measurements to evaluate the possible effect of a changing beam width over time. First, median FL values were computed for each day of GA in each of the three time-periods. Similarly, median FL values were computed for each BPD (in mm) and each MAD (in mm) in the three X periods. This allowed an assessment of whether median FL values vary over time, independent of fetal size and age. We thus controlled for potential changes in fetal growth pattern or in the time of routine ultrasound examinations. Second, to obtain a summary of the change in median FL values over the three time periods, we analyzed the data with a quantile regression model, using FL as the dependent variable and time-period as the categorical variable. Three separate analyses were done, adjusting for GA, BPD, and MAD, respectively. Third, to obtain a more detailed picture of the change in FL over time, we did the same quantile regression analyses, replacing the three time-period categories with finer categories spanning one year each. Again adjusting linearly for GA, BPD, and MAD, we obtained median FL values for each one-year category, standardized for GA, BPD, and MAD separately. - Text Source B: Økland's 2012 NTNU dr.philos. Thesis, Paper IV, MATERIALS AND METHODS, Paper IV, p. 84 (thesis pdf p. 141)
We analyzed the 41 941 FL measurements to evaluate the possible effect of a changing beam width over time. First, median FL values were computed for each day of GA in each of the three time-periods. Similarly, median FL values were computed for each BPD (in mm) and each MAD (in mm) in the three time-periods. This allowed an assessment of whether median FL values vary over time, independently of fetal size and age. We thus controlled for potential changes in fetal growth pattern or in the time of routine ultrasound examinations. Second, to obtain a summary of the change in median FL values over the three time-periods, we analyzed the data using a quantile regression model, with FL as the dependent variable and time-period as the categorical variable. Three separate analyses were carried out, adjusting for GA, BPD and MAD, respectively. Third, to obtain a more detailed picture of the change in FL over time, we performed the same quantile regression analyses, replacing the three time-period categories with narrower time-period categories spanning one year each (i.e. every year from 1987 to 2005 as a single-year category). Again adjusting linearly for GA, BPD and MAD, we obtained median FL values for each 1-year category, standardized for GA, BPD and MAD separately.
Moreover, Økland's Paper IV had been published by UOG in 2011 as: "Narrowed beam width in newer ultrasound machines shortens measurements in the lateral direction: fetal measurement charts may be obsolete" I. ØKLAND, G. BJASTAD. T. F. JOHANSEN, H. K. GJESSING, P. GRØTTUM and S. H. EIK-NES, Ultrasound Obstet Gynecol 2011; 38: 82–87. DOI: 10.1002/uog.8954. Consequently, ISUOG and/or John Wiley & Sons, Ltd. owned the copyright before Økland's 2012 NTNU dr.philos. Thesis had been publicly defended, so there were copyright issues involved given that Økland did not cite the sources for any of the many text segments she copied, verbatim, into her main thesis from the copyrighted papers included in her thesis. [Note: Paper III in Økland's 2012 NTNU dr.philos. Thesis had been accepted for publication in August 2011, but not published until May 2012, 4 months after Økland's public defense in January 2012. A similar situation existed for Paper V included in Tunón's 1999 NTNU PhD Thesis, which was identified earlier on this page.]